Nuclear Medicine
Table Of Contents
q Diagnosis
of Coronary Artery Disease
q Nuclear
Ventriculography (MUGA) Cont
q Etiologies
of a heterogeneous perfusion pattern:
q Etiologies
of decreased perfusion to one lung
q Indium
-111 Labeled Leukocytes
q Technetium -99m HMPAO - Labeled Leukocytes
q Acute
acalculous Cholecystits
q Chronic
acalculous Cholecystits
q Postcholecystectomy
pain syndrome
q Sphincter
of oddi dysfunction
q Red
Blood Cell Labeling Techniques:
q Physiology
and Function Testing
Congenital
Lesions of the Thyroid Gland
q Dyshormonogenesis/Organification
Defect
q Ectopic
Thyroid Tissue/Thyroid Dysgenesis:
q Acute
(Suppurative) Thyroiditis
q Subacute
Thyroiditis (de Quervain's Syndrome):
q Silent
(Painless/Thyrotoxic Lymphocytic) Thyroiditis:
q Chronic
Lymphocytic Thyroiditis: Hashimoto's
q Riedel's
Thyroiditis: (Riedel's Struma)
q Radiotherapy
In Non-Neoplastic Thyroid Disease
q Papillary
Thyroid Carcinoma (Roughly 66% of thyroid cancers)
q Follicular
Thyroid Cancer (10-20% of thyroid cancers)
q Anaplastic/Poorly
Differentiated: (5%)
q I-131
Ablation for Thyroid Neoplasms
q SPECT
Brain Perfusion Scintigraphy
q Pick's
Disease (Frontal lobe dementia):
q Progressive
supranuclear palsy:
Brain
SPECT for the Detection of a Seizure focus:
q Partial
Complex Seizures/Temporal Lobe Epilepsy:
q Radionuclide
Shunt Scintigram:
q Normal
Pressure Hydrocephalus (NPH):
q Communicating
Hydrocephalus:
q Acetazolamide
(Diamox) challenge test
q Preoperative
Temporary Balloon Occlusion of the Internal Carotid Artery
Cardiovascular Imaging
q Perfusion imaging
o First - Tracer must be deliverd to the myocardium
o Second – viable metabolicly active cells must be present
o If loss of cell viability or hemodynamically significant stenosis, then will have a defect.
o
Thallium 201- chloride
· K+ is major intracellular cation
·
T201 behaves like K+
· ½ lifes is 73 hours
· 95% - 69-83 KeV Mercury x-rays
· 10% -167 KeV
· 3 % 135 Kev
· 88% - extracted in 1st pass
· Peak uptake = 10- 20 minute
· 5% of dose goes to myocardium
· After several hours redistribution and equilibrium will occur.
·
Defects initially may be scar or low flow,
defects on delayed are scar
o Technetium-99m sestamibi
· Diffuses out of blood and localizes in mitochondria
· Extraction at rest is ½ of TI 201
· Uptake is rapid, clearance is long (5 hrs)
· Minimal redistribution occurs after initinal uptake, there for there is a long window (hours) to image.
· Best myocardium to background at 1-2 hrs.
· For stress, can image at 15 min
o Technetium-99m tetrofosmin
· localizes in mitochondria (lipophillic)
· Acts similar to sestamibi
o Technetium-99m Teboroxine
· lipophillic
· high extraction rate > Tl 201
· Washes in rapid with rapid washout
· Image 2- 6 mins
q Imaging protocols
o Thallium 201- chloride
· Fast for 4 hrs to reduce uptake in bowel.
·
2-3.5 mCi
· Window 69-83 KeV, can use 2nd window of 167 KeV to increase counts.
· Begin image at 10 min for poststress and rest.
· Not as good for SPECT.
o Technetium-99m sestamibi and Technetium-99m
tetrofosmin
· High quality can be obtained with planar or SPECT.
· Upto 30mCi for SPECT
· For rest image at 60-90 min
·
Same day rest and stress:
initially done with 10mCi, 2nd is done 3-4 hrs later using 20-30
mCi (account for residual activity)
·
Dual isotope (Use Tl 201 for rest)
and Tech 99m for stress. Low KeV
will not interfere with higher 167 Kev of Tech
o
SPECT
·
All porpose collimator used for Tl 201
·
Image 2-25 mins
· High
resolution for Technetium-99m
sestamibi
· May gate Tech
q Appearance of normal study
o Thallium 201- chloride
· ¯ uptake of septum near base is normal due to membranous septum
· Some lung uptake is normal, a lot may be seen in smokers ,CHF or lung disease
· Target to background better for stress
· If low liver activity, then under exercised.
· Will see uptake in liver and GI tract on resting images
· Does not cross BBB
· Thyroid, Kidneys and muscle can accumulate
o
Technetium-99m sestamibi
· Variable and ofter significant bowel activity may obscure inferior heart
· Stress and rest image the same unlike Thallium 201
· Breast can cause low counts particually along the lateral wall.
q Diagnosis of Coronary Artery Disease
o Goal - To unmask critical CAD by stressing
o Ischemia will be detected by ¯ uptake. Also ¯ wall motion
o EF should when stressed will not with ischemia
o For adequate exercise HR should be 85% of
predicted value (220-age)
o Lack of good stress is most common cause for false negative
o Stenosis up to 90% may not be seen on resting studies.
o Technique for Exercise Stress
· Beta Blockers stop 72 hrs before
· Ca channel blockers stop 48-72 hours before
· Nitrates stop 12 hrs before
· When patient reaches maximal exercise, inject tracer
· Patient maintains exercise for 30-90 sec.
· Wait 10 min to image with Tl 201
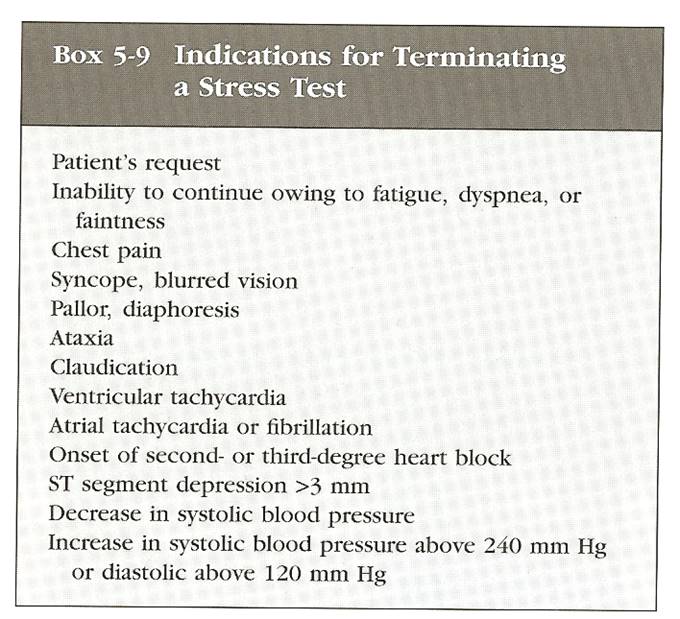
Figure 1 - Indications to stop stress
test
o Tl 201 reinjection
· 15- 35% of ischemic areas will not fill in on delayed images, scar will be overestimated
· Re-inject 1 mCi at time of redistribution imaging
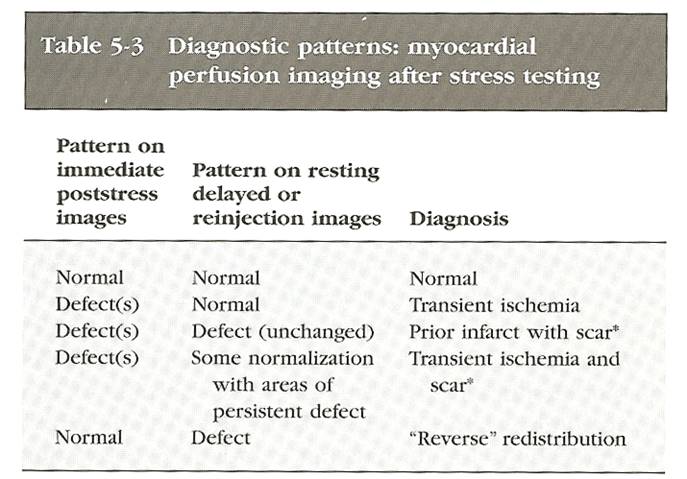
Figure 2 - Diagnostic Patterns
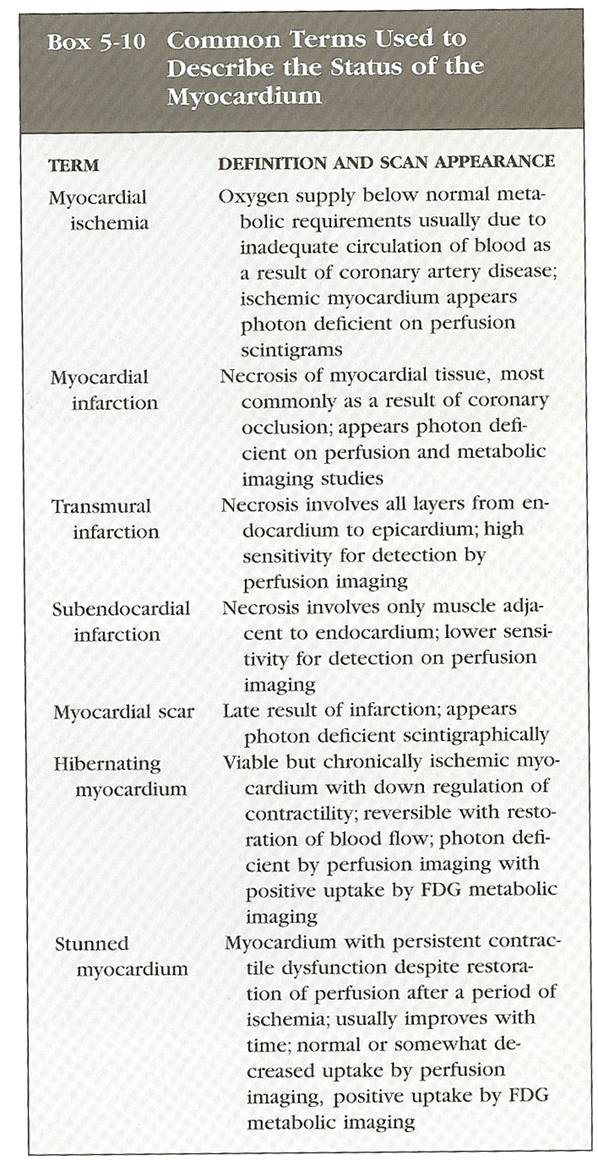
Figure 3 - Common terms
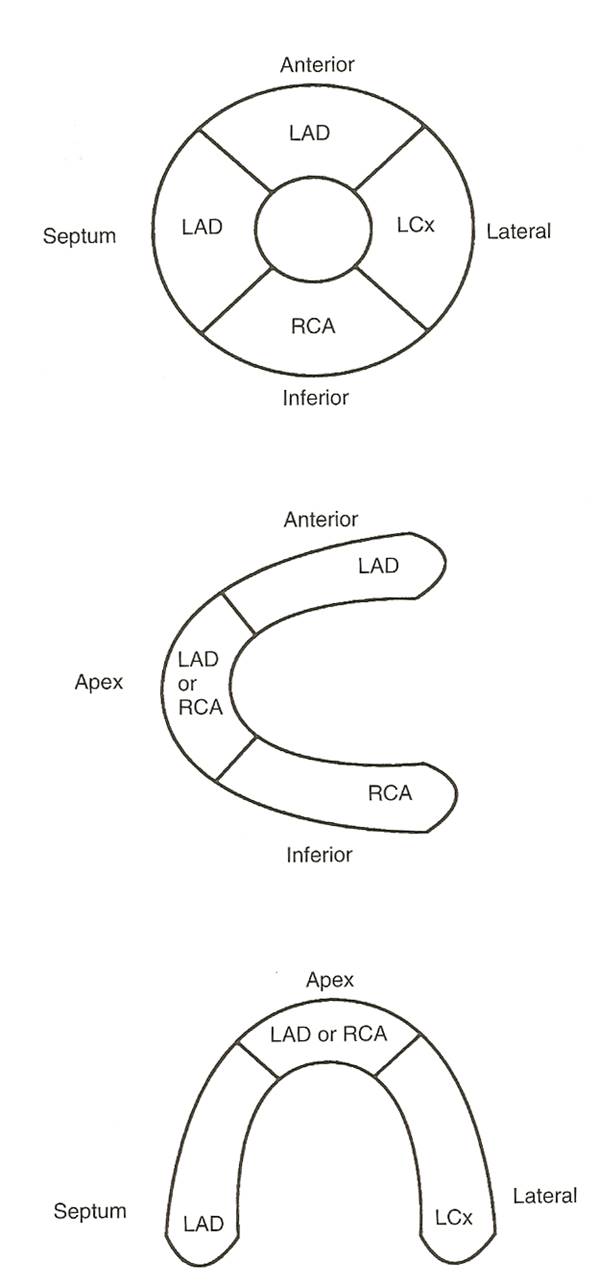
Figure 4 - Vascular territory
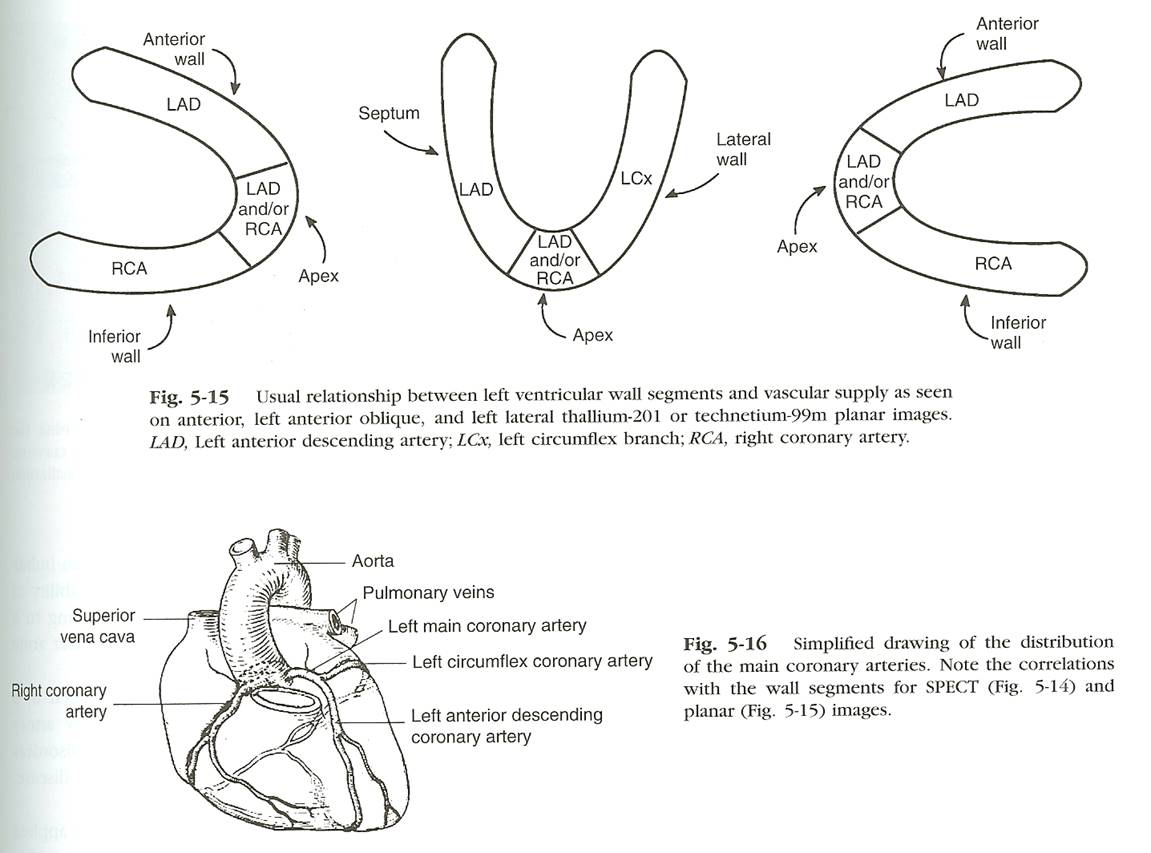
Figure 5 - Vascular territory
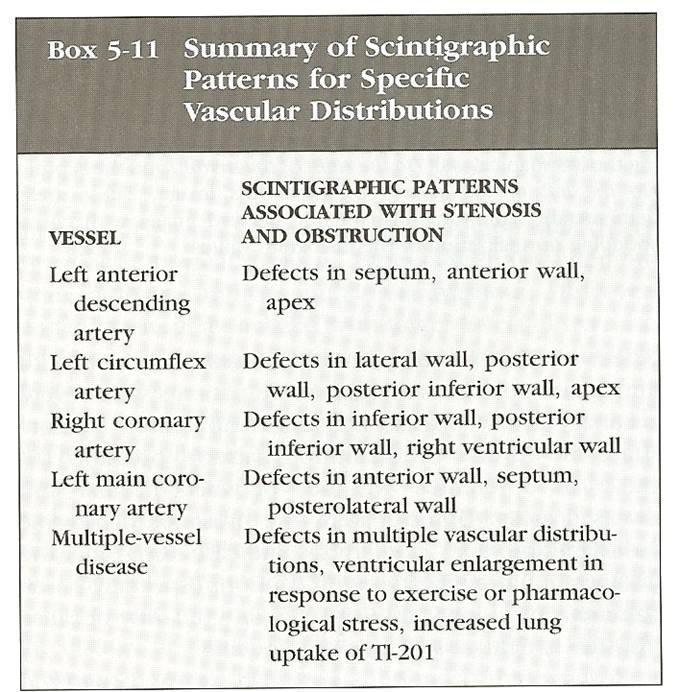
Figure 6 - Vascular territory
o Reverse redistribution - defect appears or worsens on rest – may be due to severe CAD with collateral flow but is not specific or sensitive
o
Dipyridamole and Adenisine
· Can be used to stress
· Both are potent vasodialators
· Dipyridamole blocks adenosine deaminase and augments natural adenosine. Action is longer may cause CP, SOB, NV and Low BP: Antedote is aminophylline (125-250 mg IV)
· Adenosine has advantage of very short ½ life – if symptoms develop stop infusion
· Theophylline and Caffeine (fast) can antagonize so they should be stopped
·
COPD and Asthma are contraindications
· Dobutamine can be used but causes more side effects ans is a 2nd line agent
q Diagnosis of Acute MI
o When imaged immediately sensitivity is 90% for transmural infarct.
o After 24 hrs small infarcts may not be identified
o Limited because cannot tell old defect from new with out old study.
o Also severe ischemia during angina may be cold defect bring back an image 12-24 hrs later, I may fill in. (will need to re-inject on delayed images)
o For sestamibi give initial dose when patient arrives to access at riske heart image when patient stable, then re-inject and reimage to determine effect of thromboltics.
o Stunned Myocardium
· Abnormal but still viable tissue
· Tissue in affect watershed may take up tracer but may be akinetic, if it survies wall motion will improve.
o
Hibernating Myocardium
· Severe chronically ischemic tissue which is viable but will be cold, but can be seen is active on PET
q Ventrigulography
o Used to access ventricular function
o Blood pool agents
·
Tc-99m RBC ’s
most use modified in vivo or in vitro
o First pass study
· Can be done right after stress
· Counts will not be as high
o Equilibrium gated blood pool.
· Uses R-wave gating
o Akinetic – no motion
o Hypokinetic - ¯ motion
o Dyskinetic – outward blulging during systole
o Tardokinesis – delayed motion – may be caused by ischemia or conduction abnormalities
o
EF = EDV -ESV /EDV
– need back ground – do not use the spleen.
o EF = 55-75% normal is 65%
q Acute MI
o 75% will have abnormal ejection fractions
o Patients with inferior wall MI Right ventricle should be looked at.
o Use volume overloading for pure R sided failure
q CAD
o Hallmark of ischemia is ¯ wall motion with stress and EF that does not increase or even ¯ with stress.
q Nuclear Ventriculography (MUGA) Cont
o MUGA = MUltiple Gated Acquisition scan
o Radiopharmaceutical used for the exam can be Tc-tagged RBC's
o Reasons to do
· Ejection fraction is highly accurate, probably more accurate than that obtained by any other technique.
· Second, The MUGA ejection fraction is highly reproducible.
· Ideal for detecting subtle changes in a patient's cardiac function over time
· Good for
monitoring cardio toxic chemotherapy drugs
o Acquire a short beat run to determine the average heart rate. The system then divides this R to R interval into a specified number of frames. At least 16 frames per cardiac cycle are required to calculate an accurate ejection fraction
o Arrhythmias will clearly degrade data (need to be corrected)
o Images are acquired for a 180 rotation from RAO to LPO
o Findings at Equilibrium MUGA
o Wall
Motion Evaluation
· The anterolateral and apical walls ® anterior view;
· the inferior a posterior walls ® lateral view;
· and the septal, inferoapical, and posterolateral walls on the LAO view.
· Visual inspection subjectively grades wall motion as normal, hypokinetic, akinetic, or dyskinetic
q First-Pass MUGA
o Any
Technetium-labeled agent can be used for a first-pass exam.
Pulmonary System
q Ventilation
o Xenon-133 (Beta-minus decay) (radioactive gas) disadvantage is low Kev 81, must be performed 1st to prevent down scatter from the tech 99m 140 Kev (perfusion study)
o Xenon 127 not used, to expensive
o
Tc-99m DTPA Aerosol,
· advantage can view in multiple directions after a single dose
·
0.1-0.5 micrometers
o
Technique
· Gas studies done 1st , done in 3 phaes, wash in, = phase and wash out.
· Image during all phases, no gas on wash out phase.
·
Aerosol, patient breaths in for several
minutes, dose
· Will remain in lungs for an hour
· Dose 1 mCi of DTPA assume delivered dose to lungs 25-75mCi in neb
q Perfusion
o
Tc-99m macroaggregated albumin (Tc-99m MAA )
o Lodges in percapillary arterioles, obstructing approximately 0.1% of their total number.
o typical 5 mCi dose 500,000 particles
o The number of particles used for the exam should be reduced to about 100,000 in patients with pulmonary arterial hypertension, and in those with known right to left shunts.
o 70,000 particles is necessary to obtain a diagnostic quality scan in an adult
q Pulmonary Embolism
o
A NORMAL
ventilation-perfusion scan essentially excludes the possibility of recent
significant pulmonary embolus
o In general, emboli are more frequent in the lower lobes due to the greater blood flow. Emboli are also frequently multiple (in 90%) and bilateral (in 85% of cases).
o
Defects
· Small defect (small subsegmental): Less than 25% of a segment.
· Moderate defect (moderate subsegmental): > 25%, but < 75% of a segment.
· Large defect (segmental): Greater than 75% of a segment.
o
Vascular segmental distribution:
· A segmental defect (independent of size) is a perfusion abnormality which may be triangular or rectangular shaped, periphery based, and specially located within one or several vascular segments.
· Nonsegmental defects do not conform to segmental vascular anatomy and unlikely to represent PE.
· Because the term "segmental" is also used in sizing of defects, we prefer to call defect vascular or nonvascular in appearance and distribution.
o
High Probability (80-100% likelihood for PE
·
Greater than or equal to 2 large mismatched
segmental perfusion defects or the arithmetic equivalent in moderate or large
and moderate defects. (2 mods = large)
· A high probability lung scan confirms a very high likelihood for pulmonary embolism and justifies treatment with anticoagulation .
o
Intermediate Probability (20-80% likelihood
for PE):
·
One moderate to 2 large
mismatched perfusion defects or the arithmetic equivalent in moderate or
large and moderate defects. (1 large or 2 mod), (3 mod)
·
Single matched ventilation-perfusion defect with
a clear chest radiograph
· Single ventilation-perfusion matches are borderline for "low probability" and thus should be categorized as "intermediate" in most circumstances by most readers, although individual readers may correctly interpret individual scintigrams with this pattern as "low probability".
o
Low Probability (0-19% likelihood for PE)
·
Perfusion
defects matched by ventilation abnormality provided that
there are: (a) clear chest radiograph and (b) some areas of normal perfusion in
the lungs.
·
Extensive matched V/Q abnormalities are
appropriate for low probability, provided that the CXR
is clear.
·
Any perfusion defect with a substantially larger
chest radiographic abnormality.
·
Any number of small perfusion defects with a
normal chest radiograph.
·
Nonsegmental perfusion defects (e.g.,
cardiomegaly, enlarged aorta, enlarged hila, elevated diaphragm).
· Multiple matched V/Q abnormalities, even when relatively extensive, are low probability for PE.
o
"Triple Match" in the upper and
middle zones is suggested for low probability. If seen in the lower
zone, it qualifies for intermediate probability.
o "Stripe Sign":
· A thin line (stripe) of activity (perfusion) at the pleural surface of a perfusion defect.
· associated with underlying emphysema and is likely related to spared perfusion in the cortex of the lung, the finding is considered low probability for PE
q Etiologies of V/Q Mismatch:
o Pulmonary Embolism (thrombotic, septic, air, etc.): Acute or Chronic.
o Fat emboli typically produce a mottled appearance to the scan due to the presence of many small fat emboli.
o Pleural effusion/Atelectasis: More typically, atelectasis produces a ventilatory abnormality that demonstrates normal or minimally reduced perfusion.
o Pneumonia.
o Tumor/Hilar adenopathy: Bronchi are more resistant to extrinsic compression than are the pulmonary arteries because of their rigid cartilaginous rings.
o Vasculitis/Radiation Treatment: Can reduce regional lung perfusion. Radiation treatment results in obliteration of the microvasculature. Perfusion defects from radiation are usually geometric and follow the treatment port. They are typically non-segmental. Ventilation may also be reduced in the irradiated area, but it is usually less affected than perfusion.
o Pulmonary artery atresia or hypoplasia. Segmental or branch pulmonary artery stenosis.
o Fibrosing mediastinitis can lead to central vascular obstruction.
o
AVM :
Short circuits delivery of the particulate tracer to the regional pulmonary
precapillary arterioles.
o CHF: Multiple non-segmental perfusion defects can be seen.
o Pulmonary artery sarcoma.
o Intravenous drug use: Can see bizarre perfusion patterns resulting from embolization of materials such as talc. Multiple small defects are most commonly seen, but larger defects may be noted and can occur in the absence of ventilatory abnormalities.
q Etiologies of a heterogeneous perfusion pattern:
o (Many small and medium sized defects scattered throughout both lungs.)
o CHF: May be characterized by diffuse or scattered non-segmental perfusion defects. Typically there is redistribution with reversal of the normal perfusion gradien; i.e.. upper lobes better perfused than lower lobes in an upright patient. A fissure sign refers to an oblique linear area of decreased perfusion due to pleural fluid tracking in the fissure.
o Lymphangitic carcinomatosis: Hematogenous microemboli which grow from the capillaries into the lymphatics. Contour Mapping in lymphangitic carcinomatosis appears as linear defects outlining the margins of the bronchopulmonary segments.
o Non-thrombogenic emboli: Fat, Septic, Amniotic Fluid.
o
Vasculitis.
o
Chronic Interstitial Lung Disease.
o Primary Pulmonary Hypertension. A characteristic "mottled" perfusion pattern consisting of multiple non-segmental perfusion defects with a normal ventilation exam
· The pattern is thought to be secondary to vasoconstrictive occlusion of small pulmonary arteries.
q Etiologies of decreased perfusion to one lung
o Pulmonary embolism: Thromboembolism as a cause of unilateral decreased pulmonary perfusion was previously felt to be uncommon. Unilateral decreased perfusion can be secondary to PE in up to 23% of cases .
· Generally perfusion defects are noted in the opposite lung as well. However, chronic PE has been shown to be the etiology for unilateral hypoperfusion in up to 67% of cases
o
Pulmonary agenesis: There will also be
absent ventilation and the CXR
will show a small, opaque hemithorax.
o
Hypoplastic lung (Pulmonary artery atresia):
There is usually ventilation to a small lung which demonstrates no evidence of
perfusion. On CXR the involved
lung is usually small, hyperlucent, and contains few normal pulmonary
markings
o Swyer-James Syndrome: Characterized by bronchial destruction.. In general, however, the disorder produces a more severe impairment of ventilation than of perfusion in the affected lung.
o
Pneumothorax
o
Massive pleural effusion
o
Tumor/Mediastinal mass: A central mass
can compress or occlude the pulmonary artery resulting in absent perfusion.
Endobronchial obstruction can produce hypoxic vasoconstriction.
o
Pulmonary artery sarcoma
o
Aortic dissection: Results in unilateral
right lung absent perfusion due to direct compression of the right pulmonary
artery by the intramural hemorrhage within the adjacent ascending aorta.
o
Fibrosing mediastinitis: Vessels (soft
walls) will be occluded by the progressive fibrosis prior to occlusion of the
bronchi (cartilagenous walls)
o
Shunt procedures for congenital heart disease
o
Lung transplantation with non-perfusion
of the native (diseased) lung
Skeletal System
q General
o Depicts osteoblatic activity or increased flow
o Techneium 99m MDP
· ½ 6 hrs
· Kev =140
· Dosage 15-25 mCi
· Isomeric decay
· Taken up into amorphous calcium phospahte,not hydroxyapatite
o Uptake is rapid and at 2-6 hrs 50% of dose is in bone
o Primarily excreted by kidneys
o Most image at 2-3 hrs
o Decreased tracer may be seen in low blood flow areas (infarcts) or with significant destruction (aggressive mets)
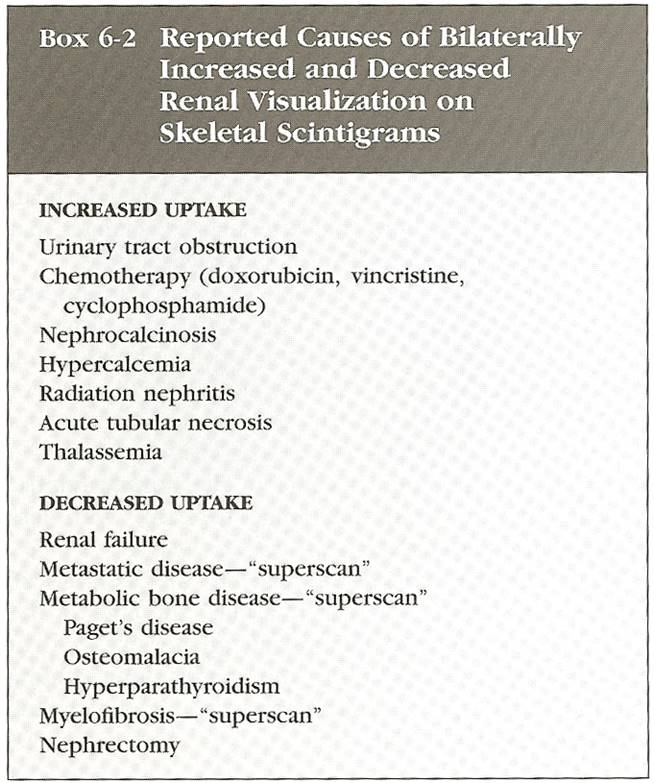
Figure 7 - Renal uptake
q Metastatic Disease
o Most epithilial tumors spread to red marrow (90%)
o Red marrow – axial skeleton, cranium, proximal portions of humerus and femur.
o 30-50% change in bone density before seen on plain film
o tracer localizes in remodeled bone not the cancer.
o
Sen = 95%
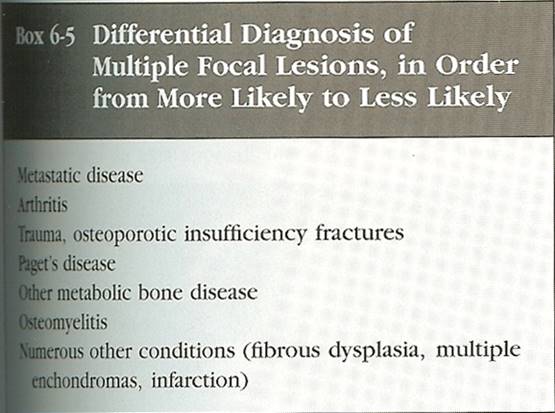
Figure 8 - Multiple focal lesions
o
Paget’s may mimic mets
o Paget’s may affect long bones and hemipelvis
o Multiple infarcts with reactive bone may also mimic mets: typically with SS
o Solitary lesion
·
Obtain plane film; if
does not answer question MRI
and/or biopsy
o Lesions in anterior rib ends are rarely mets
o Superscan
· With prostate and breast whole skeleton may be diffusely involved
· Scan may appear normal
· Absent or faint kidneys, increase in uptake of axial vs appendicular skeleton should suggest
o
Flare phenomenon
· After chemo with good response some may show flare of increased activity due to increased blastic activity of bone.
o Purely lytic lesions may be cold spot.
o Pb KTL (lead kettle) – prostate, breast, kidney, thyroid and lung common to bone
o PSA < 10 ng/ml <1% chance of mets
o Lung may affect appendicular skeleton more than others.
· May have periosteal uptake due to hypertrophic ostearthopathy
o Neuroblastoma most common tumor to met to
bone in child, Primary will take up tracer
o Other primary tumors may take up tracer
(lung, breast, colon, melanoma, metastaric colon to liver)
q Primary malignant tumors
o Avid and striking
o Typically not used ,does not answer question for surgeon
q Benign Tumors
o Osteoid osteoma – hot
o Osteochondromas, chondroblastoma and enchondroma – show spectrum may be hot.
o Enchondroma rarely demonstrate striking uptake
q Trauma
o Fractures - 80% seen at 24hrs
o Older age may show non visualization.
o Maximum at 7 days.
o Most normalize at 1 year, 95% by 3.
o Displaced fractures may be + forever.
o Radiation may show decreased activity for 6m 1 year
o Stress fractures
· Oval or fusiform in long axis parallel to bone.
o Shin splints
· Medial and Posterior
· Long increased uptake middle to distal tibia, no focal uptake like with a fracture
· Thought to be due to microscopic tears.
· Has limited uptake on early arterial images, unlike stress fracture
o Rhabdomyolysis
· Seen in marathon runners, increased uptake in thighs
· Maximum uptake 24-48 hrs resolves after 1week.
· MI in heart is the same
q Sickle Cell
o May have increased uptake in skeleton due to marrow conversion.
o May see avid accumulation in spleen from infarct and calcification
o Infarct initially cold then hot
o Sulfer colloid will be cold however need recent for comparisons to date.
q Osteomyelitis
o Staph. A most common in child
o May get increased pressure in marrow and thombosis of vessels resulting in cold spot, particularly in children (staph)
o 3 –phase
· Cellulitis does not show uptake on delayed imaging and will show venous phase hyperemia
· Oste – hot on all 3
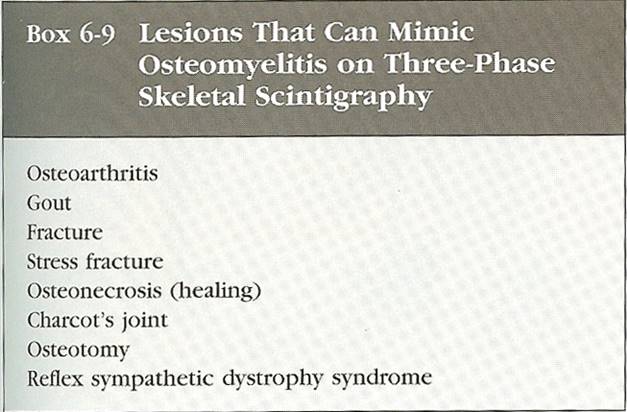
Figure 9 - Mimics of osteomylitis on 3 -phase
q Prosthesis Evaluation
o Loosening from infection may look the same
o Loosening typically increased at trocanters and tip
o Osteo typically around whole prostesis
o Negative bone scan helps rule out loosening and oste
o
Some uptake normal for
up to 1 year for of a cemented
o
Some uptake normal for
up to 2-3 years for non-cemented
o
Correlate with In
111
· May be false negative in chronic osteo
· And false + in marrow around prostesis
· + only if ( +WBC with no activity on sulfer colloid)
q Metabolic Bone Disease
o Hyperpara, hyperthyroidism, renal osteo osteomalcia and hypervitaminosis can show diffuse uptake similar to superscan (however will show increased uptake in extremities and skull and periarticular) unlike superscan
q Bone dysplasia
o Many show increased uptake
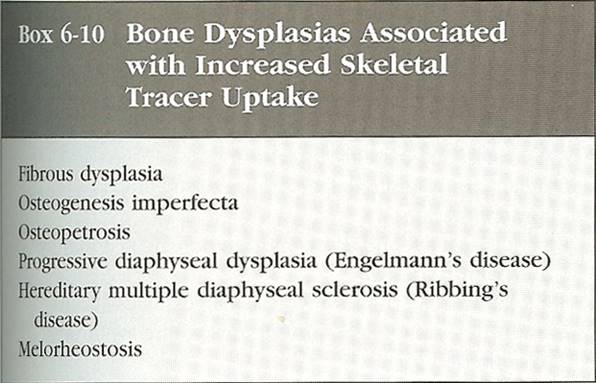
Figure 10 - Bone Dysplasia's
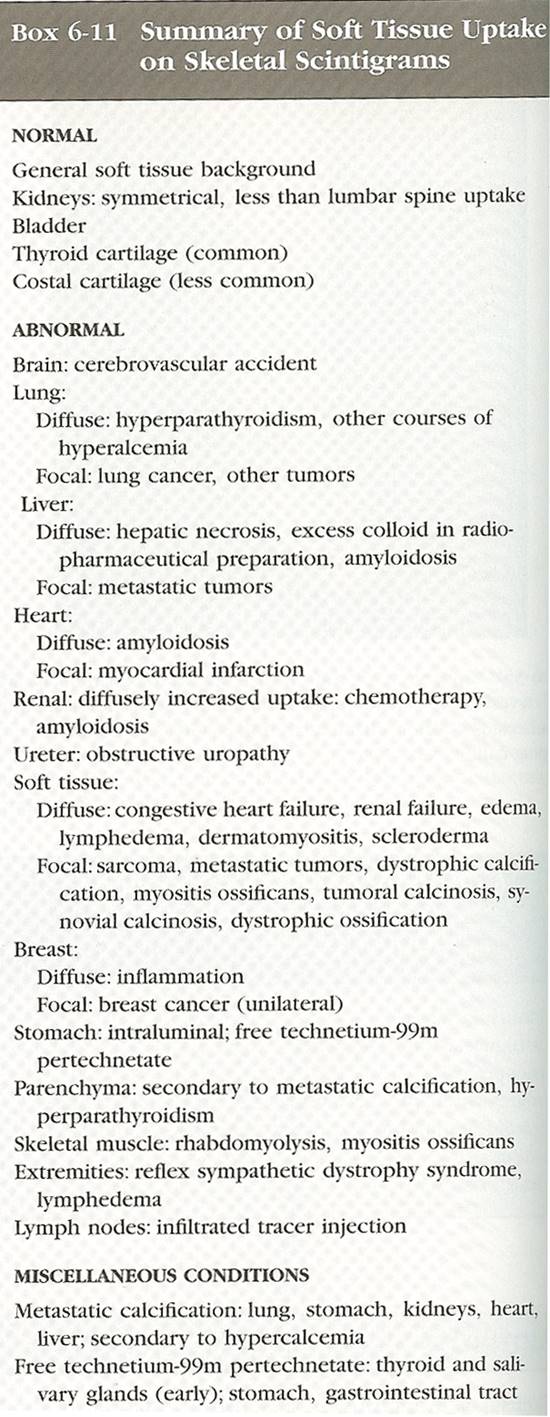
Figure 11 - soft tissue uptake
Infection and inflammation
q Gallium 67 Citrate
o ½ life 78 hours
o
circulates bound to transferrin
o Accumaltes in cells by 24 hrs
o Uptake highest in liver but also spleen ,salivary glands, bone marrow and Lacrimal gland, kidneys only faintly seen at 48-72 hrs
o Photo peaks are 93, 185 and 300
o
Increased due to blood flow and binds to
lactoferrin released by neurtrophils
o Infection 5 mCi – image at 48 hrs
o Can be used in leukopenic patients.
o
Accumaltes in all pulmonary
infections/interstitial disease pneumonia, Abcess, PCP , Sarcoid,
IPF
o
Sarcoid – lambda sign “hila and paratracheal”
panda sign “ upatake in” lacriaml submandibular and
parotid glands”
o
PCP
– diffuse uptake, may be + before abnormal CXR
o
Negative gallium and – CXR
excludes infection
o In-111 is superior for abdominal infections (GA-67 cleared by bowel)
o Good for Fever of unkonw orgin not post-op
q Indium -111 Labeled Leukocytes
o
½ life = 67 hrs
o
Typically image
at 24 hr
o
Photopeak = 173 and 247 Kev
o Dose = 500 uCi in adults
o Indium attaches to all blood cells, platlets and red blood cells mostly removed during labeling
o At 24 hrs should be no blood pool activity, if there is, it suggest high % of platlets and red blood cells are labeled.
o Most intense uptake at 24 hrs is spleen then liver and then bone marrow.
o Spleen receives the highest dose, this is a concern in peds.
o Cells removed, takes 2 hrs 75-95% efficient (in vitro)
o 50-75 cc’s of blood need indium the day before.
o
In neutropenic patients
study may be suboptimal, need WBC = 5000 however down to 3000 may
work.
o For inflammatory bowel disease image at 4 hrs because cells will slough off and not be seen at 24 hrs.
o Uptake outside of expected areas = infection/inflammation
o Ga 67 is better for TB and fungal infections.
o Antibiotics does not effect.
o False + - tracer may accumalte at sites of iatrogenic intervention (lines, tubes etc..) due to inflammation, does not have to be infection
o
Surgical wounds will show uptake for upto 10
days
q
Technetium
-99m HMPAO - Labeled Leukocytes
o Similar to Indium in distrubation but cleared hepatobilary and kidneys.
o Can do in plasma and can do immediately better photopeak.
o
Colon
o Image at 1-2 hrs for IBD 4-6 for other (osteo, etc..)
o
Better for peds due to lower radioation dose.
q Osteomylitis
o Labeled Leukocytes good when have underlying bone problem.
o Beware that focal uptake may be to abnormal distribution of marrow.
o Can perform with marrow study (sulfer colloid) distribution should be similar unless infection. On colloid typically see effect because infection displaces the marrow.
· Can also use with joint prosthesis
q Diabetic foot
o Can use Labeled Leukocytes however can see uptake in Neuropathic joints but typically not as intense.
q Bowel infection
o Use Labeled Leukocytes, not cleared by bowel like Ga 67
o Abcess – focal
o IBD follows contour of bowel
o HMPAO – is superior for IBD – can localize better.
q Pulmonary
o Can have low grade uptake in CH, atlecatais, ARDS, is non-specific.
o TB and fungal do not take up labeled WBC’s Ga 67 better
Hepatobilary System
q Agents
o Tc-99m Lidofenin HIDA
o Tc-99m disofenin
o
Tc-99m mebrofenin (Choletec)
o Have same transport and excretion as bilirubin
o Actively transported into bile system
o High levels of bilirubin will compete with tracer.
o Serum level of bilirubin > 5mg/dl may result in poor results, however may go up to 20-30
o
Mebrofenin is the best at high levels
o Target organ is large bowel.
o Delayed blood pool clearance is sign of hepatic insufficiency
o Secreted in bile at10 minutes.
o 1/3 goes to GB 2/3 goes to bowel.
o GB typically fills at 30 min up to 60 min is normal
o
Delayed filling up to 4 hrs typically in chronic
cholecytitis and also in hepatic insufficiency
o
CCK
– contracts GB and relaxes sphincter of oddi.
· Secreted from duodenum and proximal jejunum
· Released after meal, GB may remain contracted for hrs.
· Sincalide
(Kinevac) is synthetic CCK dose is
.02 µg/kg – inject over 30- 60 sec to avoid contraction
of GB neck
q Acute Cholecystits
o Fast for 3-4 hrs , if not may lead to false +
o Fasting > 24hrs may also lead to false +
·
CCK
should be given before to empty GB
o Dx made only if no filling after 3-4 hrs or 30 min after morphine
o Morphine .04mg/kg about 2 mg – infuse if GB not seen at 60 min.
o Do not give in CB duct obstruction is suspected
o Hyperalimentation and severe illness can cause false +
o Rim sign increased uptake in GB fossa seen in 25% of patients; indicates later stage such as hemorrhage or necrosis of GB.
q Acute acalculous Cholecystits
o
High mortality rate – may get false – give CCK abnormal contraction may sugest – can do tagged
WBC
q Chronic Cholecystits
o Middle aged obese women
o Gallstones usually present and will is fibrosed filled with lymphocytes
o Typically poor GB contraction
q Chronic acalculous Cholecystits
o
Will have no stones with poor GB contraction EF
< 35%
o
Pain with CCK
may be caused by Chronic Cholecystits and IBD
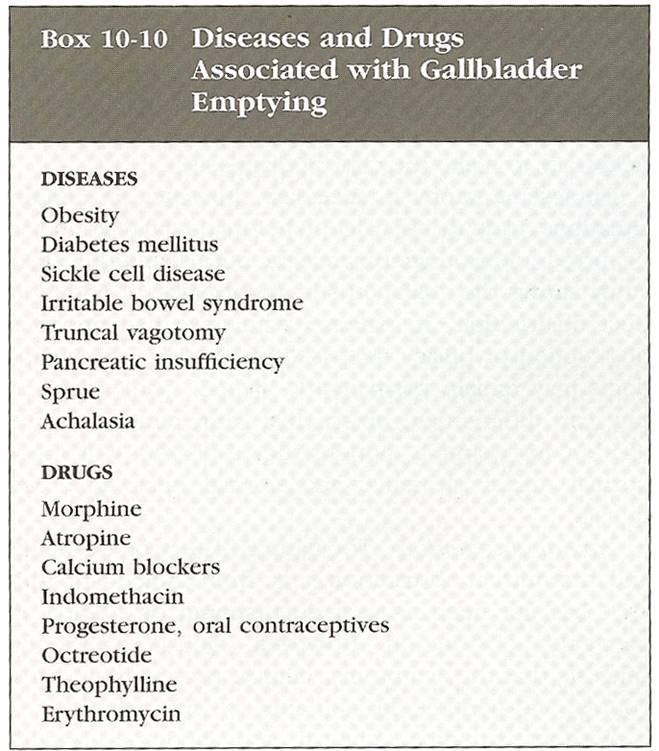
Figure 12 - GB emptying
q High grade obstruction
o Stone, Neoplasm, strcture
o May take 24-72 hrs for biliary duct dilatation
o With high grade, no excretion at 24 hrs, with partial may see delayed
o Biliary tree may remain dilated
q Partial obstruction
o
Tracer in CBD
at 1 hr suggest dx, and lack of clearing on delayed.
o
Can give CCK ,
no clearing confirms dx.
q Biliary Atresia
o Pre tx with 5mg/kg/day for 5 days.
o Lack of activity at 24 hrs is seen
q Postcholecystectomy pain syndrome
o
May be caused by CBD
stone, stricture or sphincter of oddi dysfunction
o May see findings compatible with partial obstruction
q Sphincter of oddi dysfunction
o symptoms may respond to sphincterotomy
o
is a partial CBD
obstruciton
q Other
o FNH will show uptake, adenoma will not.
o
HCC
- cold
defect -delayed may show uptake, this is
specific for hepatoma
q Tech-99m
RBC
o
Cavernous Hemangioma
· Heart and spleen most activity
· High PPV = 100%
· Use SPECT for small ones
· Planar imaging will show 3 cm or >
· Single headed SPECT 2cm or >
q Tech -99m Sulfer Colloid
o Extracted into reticuloendothelial system
o Localizes in kuppefer cells, macs of spleen and bone marrow.
o Can start within 20 min
o Most benign and malignant lesions are cold.
o In SVC obstruction collaterals will go to umbilical vein into L portal vein and may see hot spot in quadrate lobe
o Inject in lower extremity will give a normal scan
o FNH – may have increased uptake 1/3 are cold for unknown reasons.
o Budd Chiari – increased uptake in caudate, because it retains good function has on drainage
o Can be used for spleenic infarcts, accessory spleens or spleenosis
Gastointestinal System
q Gastric Motility
o Solid emptying is a Linear fashion
o Liquid is exponetional (liquids empty faster than solids)
o Mechanical causes of obstruction should be excluded by endoscopy or barium enema.
o Diabetic Gastroparesis
· Most common cause (vagal nerve damage?)
·
1 mCi of
technetium-99m sulfur colloid microwaved with 30 grams of liver pate
· Anterior and posterior static images of the abdomen were obtained at 0, 60, and 120 minutes post ingestion.
· The data were processed on the computer and the half-emptying time was calculated using the geometric mean
·
½ of contents should be gone by 120 min
· half-emptying time - (normal is 77-107 minutes for premenopausal women; 45-109 minutes for men and post-menopausal women).
q GI Bleeding
o
Tech – 99m Sulfer Colloid
· Will extrvazate at bleeding site
· 10 mCi image 1-2 min for 20 -30 min, fixed uptake not likely to be bleeding (ectopic spleen, Kidney tx)
· Major disadvantage is patient must be bleeding at time of infection.
· Good if acutely ill and unstable, fast
o
Tech -99m red blood Cell
· Advantage is if no active bleeding on initial 60-90 min films delayed imaging can be obtained
·
Can repeat at 2, 4, 6 and 24 hrs
· Activity should increase, and should see movement in GI tract
· Free Tech due to poor labeling will cause uptake instomach, which my look lke stomach or more distal bleeding: Image thyroid and salivary glands to look for uptake of free tech.
·
In pelvis, bladder, uterus
and penis may mimic bleed, lateral film is mandatory.
·
Can detect .1 CC/min, angio is 1cc/min
q Red Blood Cell Labeling Techniques:
o
In-vivo
·
Efficiency (75-85%,).
· Stannous pyrophosphate (10-15ug/kg) is injected intravenously directly into a vein
· The stannous ion (Sn+2) is the reducing agent and it diffuses into the red blood cells where it becomes bound to a cellular component.
·
After 15-30 minutes, Tc99m-pertechnetate is
injected IV and the tracer freely diffuses into the RBC 's.
·
The Tc-pertechnetate which enters the RBC 's is then reduced from its +7 valence to +4.
· Reduced technetium then binds predominantly to the beta-chain of hemoglobin (76-79%), and a small amount binds to the heme portion of the molecule (19-21%).
·
Any stannous ion present outside the RBC will reduce any free extracellular
Tc-pertechnetate and this free reduced tech will degrade images by increasing
background and urinary activity (confirm the presence of free tech by
demonstrating stomach and thyroid activity).
o
In-vitro
· Best labeling efficiency.
· The Ultra-tag kit method is now most commonly used and has a labeling efficiency of greater than 95%.
· About 3cc of the patients blood is placed in a vial with SnPYP. Sodium hypochlorite (an oxidizing agent) which cannot pass through the red cell membrane is then added to oxidize the extracellular stannous ion prior to the addition of Tc-pertechnetate.
·
Although ACD (anticoagulant citrate dextrose
solution) is preferred over heparin as the anticoagulant because it yields a
higher labeling efficiency and reduced urinary activity (see below), excess
ACD can decrease labeling efficiency by impairing the diffusion of the stannous
ion across the RBC membrane.
o
Modified in vivo: "In
vivtro" method
· This method has a labeling efficiency of about 90-95%.
· Sn-PYP is given intravenously.
· After 10 to 30 minutes (for best results) 5 to 10cc of blood is withdrawn and technetium pertechnetate (20mCi) is added.
·
After Incubating with the technetium for at
least 20 minutes, the blood is replaced. ADC
solution is the recommended anticoagulant.
q Ectopic Gastric Mucosa
o Most often in Meckel’s, less likely is duplication cyst or Barret’s
o Tc-99m pertechnetate – mucin producing cells of the gastric mucosa
o
Meckel's diverticulum
o Persistence of the omphalomesenteric (vitelline) duct at its junction with the ileum (the diverticulum therefore arises from the anti-mesenteric border).
o Complications:
· Bleeding (most common complication): Generally more common in those lesions lined by gastric mucosa (found in 95% of bleeding lesions). Ectopic gastric mucosa is found in 15-25% of Meckel's, but in about 50% of symptomatic patients [2].
· Intussusception, Volvulus
· Diverticulitis
o Tc99m-pertechnetate 10mCi is used.
o *Perchlorate should NOT be given prior to the exam as it will decrease gastric uptake of the tracer.
o Gastric concentration usually begins 5 to 10 minutes post injection, and then increases in intensity over time.
o Ectopic gastric mucosa demonstrates a similar pattern of tracer accumulation.
o A positive scan demonstrates a focal area of increased activity in the RLQ which appears at the same time as the stomach and increases in intensity in a similar manner.
o On the lateral view, the activity should be unrelated to ureteral activity.
o Cimetidine: A histamine-2 receptor antagonist which will inhibit secretion of pertechnetate by gastric mucus cells without impairing uptake. Adult patients should be pretreated with 300 mg of cimetidine p.o. Q.I.D. for 24 to 48 hours prior to the exam [
o Pentagastrin (Pentavlon): stimulates uptake of pertechnetate in gastric mucosa but also stimulates peristalsis and secretion. Do not use with Cimetidine
o Glucagon: Glucagon relaxes smooth muscle and decreases peristalsis of the stomach, duodenum, distal small intestine, and colon, should be used in conjunction with pentagastrin.
o
False Positive Exams
·
Any cause of focal hyperemia: Hemangioma
(usually multiple), AVM , Vascular
tumor
· Duplication cyst containing gastric mucosa
· Intussusception
· Inflammation/Appendicitis/Abscess
· Crohn's Disease
· Renal pelvis or collecting system activity
· Uterine Blush: Menstruating females
· Retained Gastric Antrum:
o
Retained gastric antrum syndrome
· occurs in patients who have undergone partial gastrectomy with a Billroth II anastomosis.
· The gastrin secreting cells of the antrum are no longer inhibited by gastric acidity and the resultant increased acid output by the stomach leads to recurrent marginal ulceration.
· Normally, there should be no activity identified in the region of the pylorus/duodenum in these patients. Retrograde filling of the afferent loop can be seen on cinematic display of acquisition images.
o
Barrett's Esophagus
·
Accumulation of Tc-pertechnetate in the lower
esophagus after I.V. administration is considered a positive examination for
the mucous secreting cells of Barrett's mucosa.
·
Unfortunately, swallowing of free
Tc-pertechnetate in the saliva and reflux of gastric activity can cause
significant problems with scan interpretation.
·
Currently, scintigraphy plays no definitive role
in the evaluation of patients with suspected Barrett's esophagus.
Genitourinary System
q Basics
o Cortex contains glomeruli
o Medulla = colleting tubules and loops of henle
o Receives 25% of cardiac output
o 20% of blood flow is filtered through kidney’s
o High renal plasma flow (RPF) and efferent artery maintain pressure gradient
o Remaining 80% not filtered is actively secreted.
o Tubules actively reabsorb water and (glucose, amino acids etc…)
o
Glomerular filtration
· Should no be reabsorbed or secreted.
· Should not be protein bound
· Tc-99m DTPA (diethylenetriamine pentaacetic acid) is good.
· 20% of renal function
o
Tubular secretion
· 80% of renal function
·
Tc-99m MAG 3
(mercaptylacetyltriglycine)
o
Cortical binding
· Tc-99m GH (glucoheptonate)
· Tc-99m DMSA (dimercaptosuccinic acid)
· Bind to proximal tubular cells in cortex
· Allows good functional imaging in the cortex
·
Good in pediatrics to diagnose scaring of
pylonephritis, will have cold defect.
o
Tc-99m DTPA
· 20 mCi good blood flow images
· Can be used for evaluation of suspected obstructive uropathy.
· If free tech will see uptake in thyroid, salivary glands and stomach.
· Peak cortical uptake occurs at 3-4 minutes.
·
Clearance is a function of normal GFR
· Normally 120ml/min
·
½ life is 2 ½ hrs.
· By 5 minutes tracer appears in collecting system.
· Bladder activity at 1-15 minutes
· ½ time of renal clearance is 15-20 minutes
o
Tc-99m MAG 3
(mercaptylacetyltriglycine)
· In patients with normal renal function, glomerular or tubular agents can be used and provide similar information
· For renal insufficiency tubular agents are clearly better due to there high extraction efficiency.
· High first pass extraction.
o Tc-99m GH (glucoheptonate) Tc-99m DMSA (dimercaptosuccinic acid)
· Prolonged and stable retention in kidneys.
· Cortical images obtained 1 ½ - 2 hrs after injection
q Renal imaging Techniques
o
Similar protocols for dynamic imaging can
be used for Tc-99m GH, DTPA and MAG 3
o Patients should be hydrated, if dehydrated may result in delayd uptake and excretion.
o Typcail patient is supine and posterior imaging is done.
o Anterior is used for transplants
o
Dose
· Tc-99m GH – 20 mCi
· DTPA – 15 mCi
·
MAG 3
- 8 mCi
o 60 second flow study or perfusional phase
o Followed by 25-30 min dynamic functional imaging demonstrating uptake and clearance
o
Interpretation
· Flow phase – flow to kidneys 4-6 sec after aorta seen – delay on ones side suggest decreased perfusion
· Cortical Function phase (1-3 min) – can look at image and judge uptake, poor functioning kidney will show less at beginning and more later as good kidney clears tracer.
· Clearance phase – calyces and pelvis begin to fill at 3 min, may not see normal ureters.
o
Renal cortical imaging
· Scarring vs infection shown as a defect.
· No dynamic imaging with DMSA
q Computer Processing
o
Dynamic renography
·
Can obtain 60 sec and 25-30 min renograms
· Renal Blood Flow –
o For 60 sec ROI on kidney and Aorta
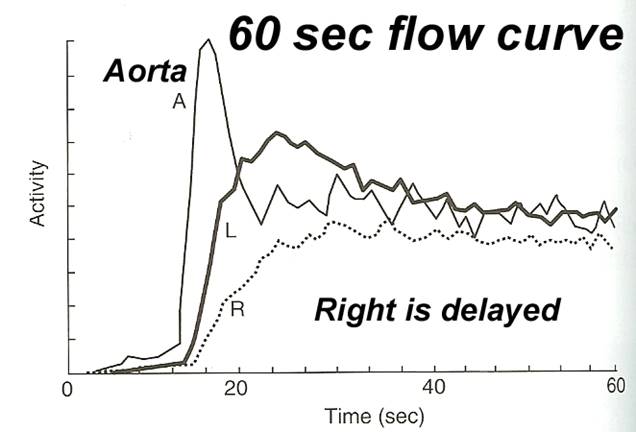
Figure 13 - 60 sec curve wih decreased perfusion in right kidney
.
· Renal Cortical function –
o generated for 25-30 min manifested by uptake and excretion (balance between 2) with 3 phases (blood pool, uptake and excretion.)
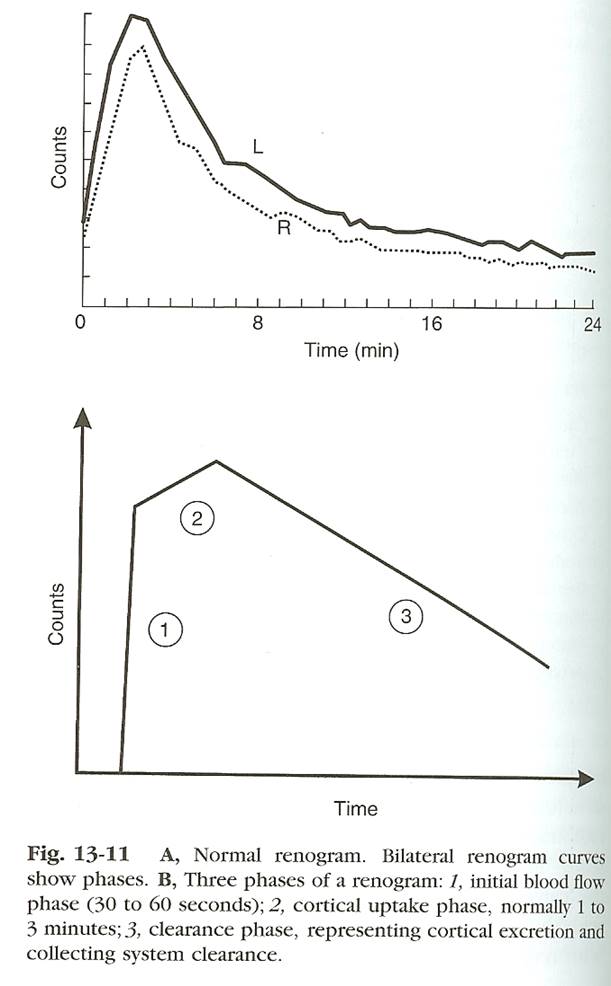
Figure 14 -
· Differential function –
o 45-55% is normal –
o obtained by cortical uptake counts at flow phase (1-3 min).
o = (Total counts of 1 kidney)/both counts
o
Filtration rate and plasma flow
·
GFR
is 100ml/min
q Renovascular
HTN
o Caused by stenosis
o Of referred patients 2-4% will have.
o May show decreased flow on stenotic side, however this is not sensitive
o
Stenotic side will show delayed uptake and
clearance
o This is not specific and can be seen in other renal dysfunction.
o
Angiotensin –converting enzyme inhibition
renography
· GFR ¯
→ Renin →angiotesninogen →
angiotensin I in liver → angiotensin II in lungs by ace
· angiotensin II – powerful vasoconstricter, constrict efferent arteriole (away) in kidneys keeps pressure up.
·
ACE
inhibitors block angiotensin I in liver → angiotensin II in lungs , will decrease GFR
·
Captopril
o Typically study done with and without
o Typically done with ace inhibitor 1st, if normal then you are done, if not then need a baseline on a separate day.
o Lasix is often given with tracer to ensure clearance.
o Diagnostic pattern – Classic pattern is abnormal ace study with normal base line.
o If asymmetry on baseline, captopril will result in greater asymmetry
o With DTPA (glomerlar agent) will show ¯ absolute or relative uptake
o
With MAG
3 will show will have cortical retention
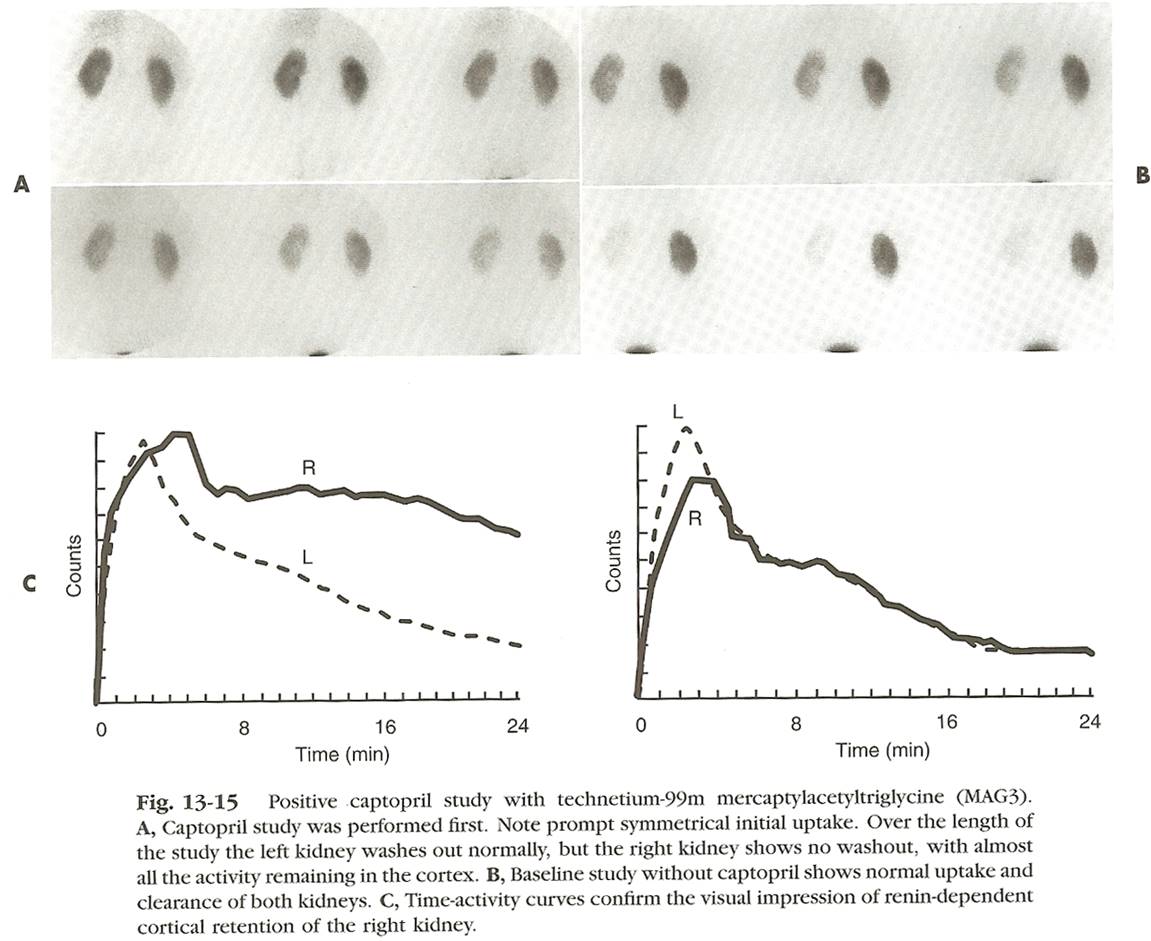
Figure 15 - + captopril, returns to normal with no ACE
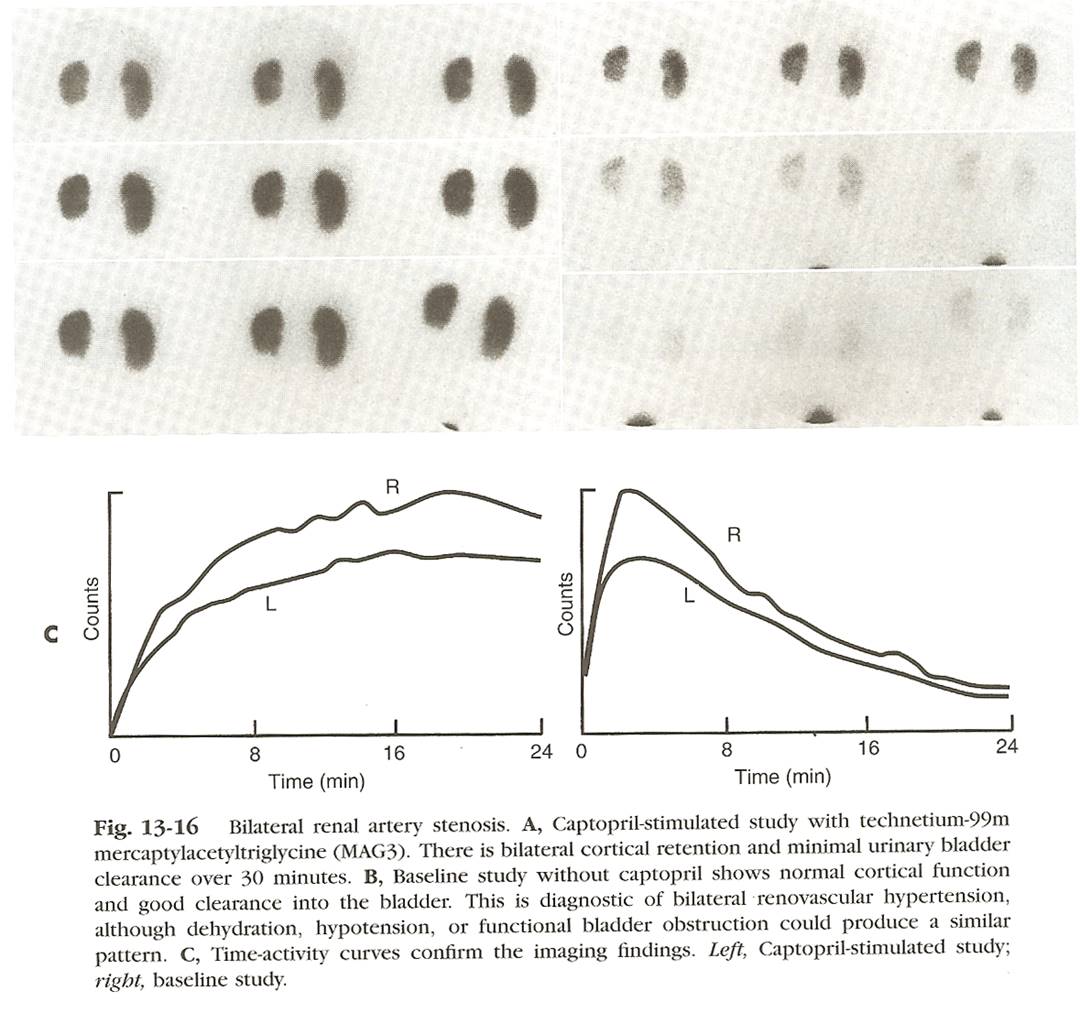
Figure 16 - Bilateral Renal artery Stenosis
q Urinary Obstruction
o Obstruction vs dilatation important to know.
o High grade obstruction for 1 week will lead to loss of some renal function
o Low grade may go on for months or even years with no problems.
o
Diuretic renography
· Principle is that delayed retention in dilated/non obstructed kidney will show wash out with diuretic. Obstruction will show much less wash out.
·
MAG -3
is agent of choice
· Furosimide is typical agent used.
· Use IV inject over 1-2 min, onset is 30-60 sec with maximal effect at 15 min.
· Empty Bladder, it may prevent wash out
·
Different protocols but standard 1st
use routine 25 min dynamic imaging, then additional acquisition after lasix for
20 min
· High grade (chronic) – may show no function
· High grade (non- chronic)– may show decreased function with no clearance
· Low grade – dilated collecting system which pools with little pelvicoclyceal clearance
· In non-obstructed kidney – will clear after lasix
· With severe hydro or poor renal function, there may be delayed wash out with lasix.
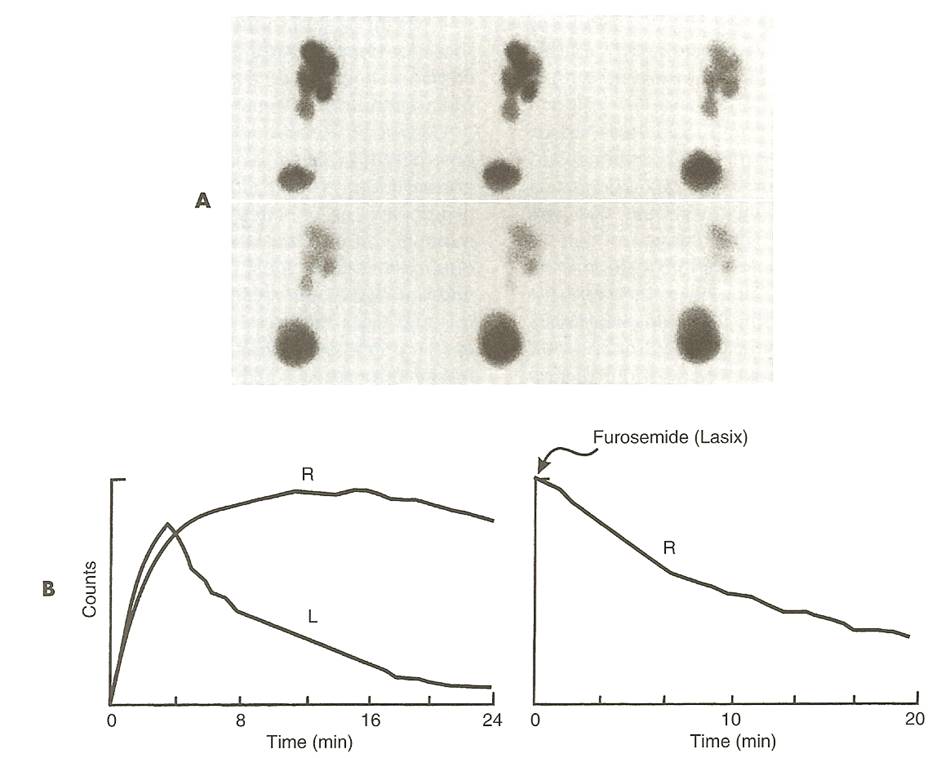
Figure 17 - Non -obstructive hydronephrosis, Clears with lasix
·
Obstruction
o Washout ½ time < 10 min no significant obstruction
o Washout ½ time > 20 min is consistant with obstruction
o Between 10-20 min is indeterminate.
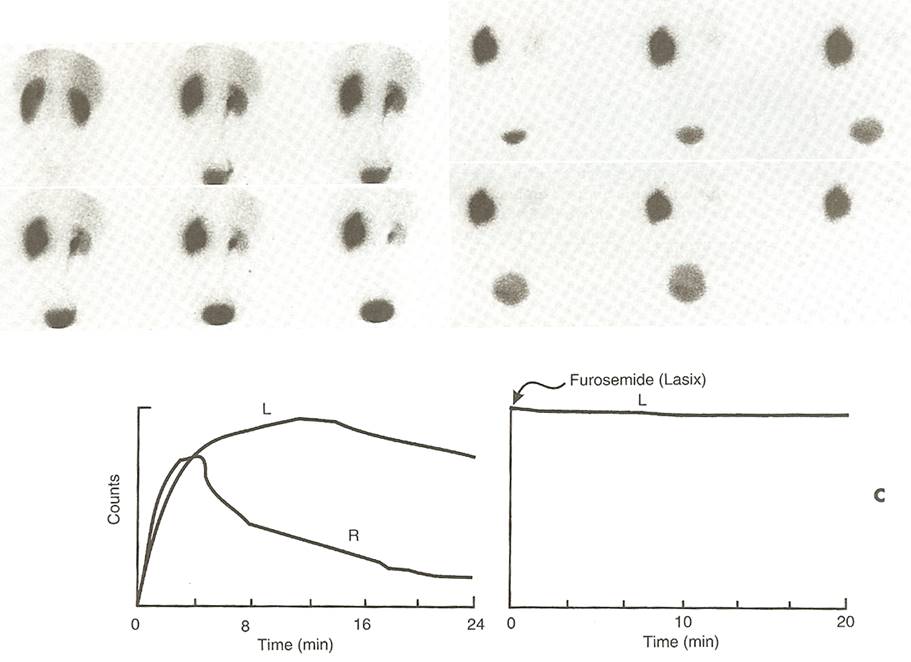
Figure 18 - Obstructed Kidney with no clearance after lasix
· Pit falls may occur in Neonates – due to immature kidneys, may be followed.
q Renal Transplant
o ATN – earl long time from donor (dead) to patient, will show good flow with no exretion in 1st 24 hrs. resolves in 1-2 weeks
o Hyperacute rejection –turns bleu in OR – rare will show no flow to kidney.
o Will see same picture with arterial or venous thrombosis (bad because no collaterals)
o Acute rejection – 5-7 days upto 3 months hall mark is decreased perfusion and function.
o Chronic – occurs months to years after tx, decreased perfusion and urine formation
o Other –arterial stenosis, urinoma, obstruction and Lymphocele (2-3 months)
q Radionuclide Cystography
o More senitive and less radiation (50-200 times)
o Resolution of refulx in 805 of patients
o
Indirect- Patient waits till bladder
fills then obtain a pre, then dynamic images will patient voids Can use DTPA
or MAG 3
o Direct- most often used, use DTPA or Sulfer colloid, child must be cathed image while filling, voiding and pos void
Thyroid
q Physiology and Function Testing
o
Thyroid Releasing Hormone (TRH ) is a peptide hormone synthesized in the
hypothalamus and passed through the hypophyseal portal venous system.
o
Anterior pituitary, TRH stimulates synthesis and release of Thyrotropin
(TSH ).
o
TSH
stimulates the thyroid.
o
Thyroid Hormone Synthesis
·
4 basic steps:
· Iodide trapping - iodide is actively transported into the thyroid gland
·
Organification - the enzyme thyroid
peroxidase forms inactive (MIT) and (DIT ).
MIT and DIT are incorporated into
the soluble protein thyroglobulin which is stored as colloid in the
follicular lumen.
·
Coupling - the enzyme thyroid peroxidase
catalyzed the coupling of MIT + DIT
to form triidothyronine (T3) and the coupling of DIT
+ DIT to form thyroxine (T4).
· Release - proteolysis of thyroglobulin produces the active hormones T4 and T3, which are then secreted into the blood.
· 90% of the released thyroid hormone is in the form of T4, and 10% in the form of T3.
o
Thyroid Hormone Transport/TBG
· 99% of thyroid hormone is carried in circulation firmly bound to three major binding proteins: thyroid binding globulin (TBG), transthyretin (TTR, formerly called thyroxine binding pre-albumin - TBPA) and albumin
· TBG made in liver, Estrogen Effects –(pregnancy, oral contraceptives), Infectious Hepatitis ,Biliary Cirrhosis: increase TBG and total T4, but free T4 is unchanged
· Decrease TBG - Androgens and Anabolic Steroids, Large doses of Glucocorticoids, Nephrotic Syndrome, Major Systemic Nonthyroidal Illness, Active Acromegaly, Chronic Liver Disease ,Drugs - dilantin, tegretol ,Genetic Determination
o
TSH
is 0.5-5.0 mU/L
o Fetal thyroid does not concentrate iodine during the first 12 weeks of gestation.
o Beyond this point, iodine uptake increases progressively until term.
q Radionuclides
o
Iodine-123
·
decays by electron capture,
·
half-life of 13.6 hours, and a gamma
energy of 159 keV.
·
produced in a cyclotron by either one of two
methods:
· Dose -200-400 uCi
·
Indications - agent of choice when
evaluating substernal goiters because there is usually substantial
mediastinal blood pool activity associated with Tc-pertechnetate.
·
Maximal count occurs at 6 hours.
·
Acquired images at 4 hours,uptake
values are determined at 4 and 24 hours. At Emory images are acquired at 24
hrs and uptake is as well.
o
I-131
·
is reactor produced.
·
Dose
o
Diagnostic: 2-5 mCi po for whole
body for following a patient with thyroid carcinoma.
Therapeutic: 80-150 uCi per gram of thyroid tissue for Graves'
disease
o 100-200 mCi for thyroid carcinoma ablation in thyroid neoplasm
· Thyroid hormone should be discontinued for several (2-6) weeks in advance of study or treatment.
·
A serum TSH
level is very helpful to gauge the adequacy of thyroid hormonal withdrawal.
·
Unless the TSH
level is increased, the validity of an I-131 body scan, especially if it is
normal, should be questioned.
·
Indications
o a very high radiation dose to the thyroid, 90% of which is the result of beta decay (see below).
o I-131 is not the tracer of choice for imaging applications, except in the case of delayed imaging for thyroid carcinoma metastases or mediastinal masses.
o
Technetium-99m Pertechnetate
·
Trapped by the thyroid gland in the same
manner as iodine (an active transport mechanism).
·
After trapping pertechnetate slowly
"washes" from the gland- it does NOT undergo organification.
·
Peak thyroid activity 20 and 40 minutes
·
Only 2-4% of the administered dose is trapped in
the thyroid. Pertechnetate is secreted in human milk (discontinue breast
feeding for 48 hours after dosing) and also
crosses the placenta to accumulate in the fetus.
·
The uptakes of radioiodine and pertecnetate are
both decreased by pool (iodinated contrast, dietary, or the antiarrhythmic
agent amiodarone).
· Dose -3 mCi intravenously.
· Reported cases of thyroid carcinomas that are capable of trapping but not organifying iodine.
· It is possible to have a warm or hot nodule on a Tc-99m scan that would be cold on I-123.
· Any patient with a non cold nodule on a Tc-99m scan should be repeated with I-123 to avoid this disparity.
· Cold nodules with Tc-99m scan will inevitably be cold with an I-123 scan.
· Indications (preferred imaging agent when)
o Patient has been taking thyroid blocking agents (Propylthiouracil). Thiouracil blocks oxidation and organification of iodide following its uptake by the thyroid gland, but will not interfere with trapping of pertechnetate.
o Patient is unable to take medication orally
o The study must be completed in < 2 hrs
o thyroid function (uptake studies) are not necessary
q Nuclear Imaging Tests
o
Radioactive Iodine Uptake Test (RAIU)
· %
Uptake= [(net neck counts - net thigh counts)x 100]
/(net standard counts)
·
(normal = 10 - 30 %).
· In "true hperthyroidism" - RAIU uptake will be high while thyrotoxic patients with thyroiditis or who abuse thyroid hormones will have a low RAIU
o
Pregnancy is an absolute contraindication to
thyroid scanning, especially after the 12th week of gestation when the fetal
thyroid begins to trap iodine.
Congenital Lesions of the Thyroid Gland
q Dyshormonogenesis/Organification Defect
o Results from a deficiency or absence of one or more of the enzymes involved in thyroid hormone synthesis or secretion.
o Most common enzyme abnormality is absent or insufficient thyroid peroxidase activity
o With this type of defect iodine will be trapped, but not organified.
o
Patients with peroxidase deficiency frequently
have an enlarged gland (although it may be normal sized), an elevated TSH
o Pendred's syndrome - associated with a familial goiter and deafness or hearing.
q Ectopic Thyroid Tissue/Thyroid Dysgenesis:
o Can be lingual, substernal, or pelvic/ovarian teratoma (struma ovarii).
o Pertechnetate is generally not useful for imaging the substernal area
q Lingual Thyroid
o Extreme failure of thyroid migration.
o may provide adequate amounts of thyroid hormone, or may fail in early childhood
o In over 70% of patients with a lingual thyroid, no other thyroid tissue can be found in the neck [1].
o Clinically resembles a thyroglossal duct cyst. Symptoms are typically related to mass effect and include dysphagia and dyspnea.
o There is an association with thyroglossal duct cysts.
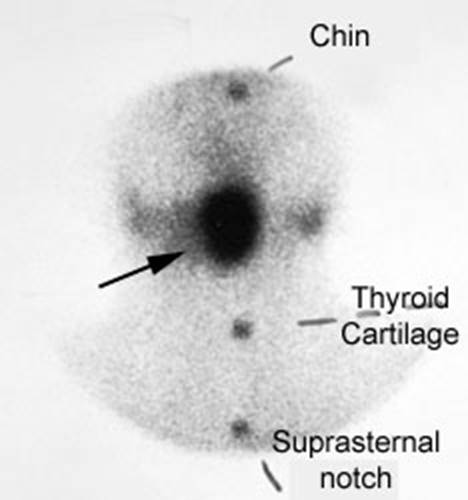
Figure 19 - Lingual thyroid
q Thyroglossal duct cyst
o Appear in the midline along the migratory path of the embryologic thyroid gland, anywhere from the foramen cecum at the base of the tongue to the lower neck.
o Vast majority of patients with thyroglossal duct cysts have normal thyroid scans.
o Surgery is contraindicated if functioning thyroid tissue is demonstrated in the mass.
o The cyst may become infected, and rarely a papillary thyroid carcinoma may develop within a thyroglossal duct cyst.
q Substernal Thyroid
o I-123 is the preferred imaging agent due to mediastinal blood pool activity with Tc-99m.
o Most intrathoracic goiters demonstrate anatomic continuity, but not necessarily functional continuity with cervical thyroid tissue.
q Hemiagenesis
o Females are affected more than males (3:1).
o The left lobe of the gland is absent in about 80% of the cases
o The remaining lobe is hypertrophied, but normal in shape
q Acute (Suppurative) Thyroiditis
o Rare, and life threatening infection (abscess) of the thyroid gland.
o Most commonly a bacterial infection caused by Strep., Staph., or Pneumococcus.
o More localized
o Most patients are clinically euthyroid
o RAIU is usually decreased
o Can spread directly along the fascial planes of the neck or hematogenously producing a systemic sepsis.
o Treatment is multifaceted and consists of surgical drainage, tracheostomy and antibiotics.
q Subacute Thyroiditis (de Quervain's Syndrome):
o Characterized by lymphocytic, granulomatous, and foreign body giant cell infiltration.
o probably has a viral etiology.
o As the thyroid becomes damaged, hormone leaks out into the blood producing thyrotoxicosis. At this point, the thyroid gland has essentially stopped functioning because of the inflammation, and iodine uptake will be low.
o After hormone production resumes, the patient generally recovers without further complications.
o Females are affected more than men (5:1).
o Patients often have a preceding upper respiratory tract infection 2-3 weeks before.
o Patients typically recover fully without residual thyroid dysfunction (Only about 5% will be left with some degree of thyroid dysfunction)
o Progresse
through a series of phases that dictate the clinical and scintigraphic
findings. Imaging
o
On scintigraphic examination
· early subacute thyroiditis there is typically poor visualization of the entire thyroid. Single or multiple hypofunctioning areas are occasionally seen as the disease can be focal and present as a cold area/nodule.
· Increased radioactive iodine uptake is seen during the hypothyroid phase (late) of the disease.
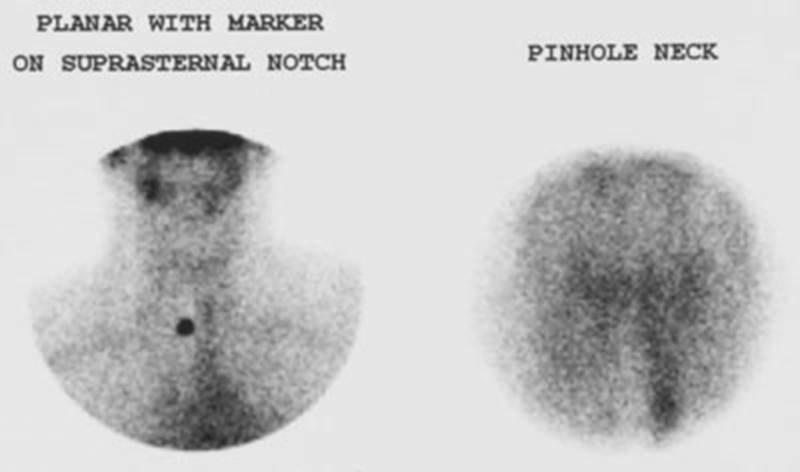
Figure 20 - Presented with symptoms of
hyperthyroidism. The
T4 level was elevated and the scan was done to exclude
q Silent (Painless/Thyrotoxic Lymphocytic) Thyroiditis:
o Autoimmune disease that is characterized by elevated levels of thyroid peroxidase antibodies and thyroglobulin antibodies
o It is a form of lymphocytic thyroiditis
o Patients typically have symptoms of thyrotoxicosis, but without a tender or painful thyroid associated with subacute thyroiditis (although the thyroid can be enlarged in 50-60% of affected patients [1]).
o
T3 and T4 are elevated, the TSH is decreased, and the RAIU is decreased.
o
ESR
is normal and there is no history of preceding URI .
o The condition will generally resolve spontaneously [2]. The thyrotoxicosis is usually mild to moderate and lasts for 1 to 4 weeks (up to several months [2]), followed by a euthyroid period, and then transient hypothyroidism [1].
o
Thyroid scintigraphy reveals markedly
decreased glandular activity
q Postpartum
thyroiditis
o 5 % of post-partum patients.
o generally considered to be a subtype of silent thyroiditis that appears 2 to 12 months after delivery (most commonly between 4 to 6 months).
o The course and findings are similar to silent thyroiditis
o In contrast to the recovery of normal thyroid function that is expected in most patients with silent thyroiditis, between 23-33% of patients with painless thyroiditis will become permanently hypothyroid.
q Chronic Lymphocytic Thyroiditis: Hashimoto's
o Hashimoto's thyroiditis is also known as chronic autoimmune thyroitditis
o It is an autoimmune disorder characterized by goiter and lymphocytic infiltration [1]. familial predisposition.
o Antimicrosomal (anti-thyroid peroxidase [TPO] antibodies) are the most commonly found- 90-95% of patients [1] and are markedly elevated during the acute phase of the disorder.
o Unfortunately, anti-TPO antibodies are not specific
o Early on, there is mild, diffuse lymphocytic infiltration of the thyroid.
o Late in the disorder there are plasma cell infiltrates, fibrosis, and destruction of the gland.
o Hashimoto's is the most common inflammatory thyroid disease (accounting for about 85% of cases of thyroiditis).
o Most frequent cause of goiterous hypothyroidism in adults.
o Females are affected more than males (9:1).
o ages of 30-50 years, but the disorder may be seen at any age.
o Patients with Hashimoto's thyroiditis develop other autoimmune disorders with higher frequency and are at increased risk for developing B-cell lymphoma of the thyroid.
o Initially, the gland enlarges
o hormone levels tend to be maintained until late in the disorder, at the expense of an enlarged gland..
o Clinically patients present with gradual painless thyroid enlargement (firm rubbery gland).
o RAIU is typically normal until late in the disease course, but may be elevated in patients with Hashitoxicosis.
o Eventually, as thyroid tissue is replaced by fibrosis, serum hormone levels will fall and patients become hypothyroid.
o About 20% of patients are hypothyroid at presentation (20%).
o
Pain is rare, but if present, may mimic subacute
thyroiditis (SAT ). The RAIU will
aid in differentiating the two conditions as RAIU is generally normal in
Hashimoto's, but is decreased in SAT .
o Thyrotoxicosis is also rare (4%) and may be related to the release of thyroid hormone during the early stages of the disorder.
o Hashitoxicosis: Hashimoto's thyroiditis can also manifest as an acute mild to moderate hyperthyroidism in 3-5% of cases.
o RAIU is normal or elevated.
o The hyperthyroidism is typically self-limited and resolves spontaneously over a period of weeks to several months [1].
o
Imaging
· Variable.
· Multinodular goiter appearance is common with multiple (40%) or single (30%) cold defects. There can be diffuse, uniform increased tracer activity, to a coarse patchy distribution of tracer, or focal/diffuse absence of activity.
·
The pyramidal lobe may appear prominent due to TSH stimulation. A normal scan is seen in about 8%
of patients.
· Until thyroid reserve is disrupted, patients typically have a normal RAIU.
q Riedel's Thyroiditis: (Riedel's Struma )
o Rare condition.
o In this disorder, there is painless replacement of the thyroid by dense fibrous tissue and which may also involve adjacent soft tissues of the neck and is often mistaken for cancer.
o Between 30 to 40% of patients will progress to hypothyroidism as the infiltrative progress involves the gland.
o Occur in 4-15% of the adult population
o The major challenge that faces a clinician is to determine whether a thyroid nodule is benign or malignant.
o Hyperfunctioning nodules are more likely to have a benign process.
o Thyroid nodules are found by US in 30-50% of patients [12,15].
o The prevalence of nodules also seems to increase with age.
o Hyperechoic solid nodules are usually benign (96%), but sclerosing papillary neoplasms can also have this appearance.
o Mixed lesions represent solid lesions which have undergone variable degrees of cystic degeneration and are benign in 85% of cases.
o Cystic lesions that are completely smooth walled and anechoic are almost always benign. Iso- or hypoechoic lesions may be benign or malignant.
o Since thyroid ultrasound cannot determine if a nodule is benign or malignant, it is not routinely recommended in the initial evaluation of a thyroid nodule.
· May be useful to guide fine needle aspiration biopsy
o Almost all solitary thyroid or dominant nodules need to be biopsied.
q Cold Nodule
o A cold nodule reflects lack of organification.
o The great majority of solitary thyroid nodules are cold (hypofunctioning), but only 10 to 25% of these are malignant
o Thyroid cancers appear as cold nodules due to altered iodine metabolism
o Recommend FNAB on dominant nodules in patients with MNGs
o However, cancer can occur in non-dominant nodules and multinodularity of a goiter should no longer be considered an indicator of probable benign disease.
o
Differential considerations for a cold nodule
include:
· Benign: Roughly 80% of cold nodules are benign leions)
·
1- Simple Cyst
o
True epithelial lined thyroid cysts are RARE . More are degenerating adenomas or colloid nodules.
·
2- Adenomatous hyperplasia (Colloid
cyst/Non-functioning Follicular Adenoma)
o colloid cyst is a localized colloid filled follicle.
o Most common cause of a hypofunctioning thyroid nodule
o May be solid, but areas of hemorrhage or cystic degeneration are commonly seen. Patients usually present with an enlarging thyroid nodule.
o Rapid enlargement and pain is associated with intralesional hemorrhage.
o On aspiration, the cyst fluid will have high T3 and T4 levels.
· 3- Focal Hemorrhage
· 4- Inflammatory:
· 5- Parathyroid Adenoma
·
Malignant (20%)
o 1- Thyroid carcinoma
o 2- Parathyroid adenoma/carcinoma
o 3- Thyroid Lymphoma
o 4- Metastatic Disease
o
Risk factors for malignancy
· History of XRT to head and neck as an adolescent or child Risk 30% if there is a history of XRT.
· Adenopathy (Regional)
· Age - Less than 20 (about 2 fold increased risk [3]) or over 60 years (about 6 fold increased risk)
· Male
sex
· Evidence
of local invasion
· Size of nodule greater than 4 cm
· Family history of thyroid cancer
q Hot Nodule
o A toxic nodule is an autonomous nodule that produces enough thyroid hormone to cause thyrotoxicosis.
o Differential considerations for a hot nodule include:
· Benign
hyperfunctioning follicular adenomas
o
Accounts for almost all hot nodules, 50% are
autonomous- i.e.: TSH independent.
Patients can be euthyroid or hyperthyroid
Figure 21 - autonomously functioning nodule within the lower pole of the right lobe of the thyroid gland. The remainder of the thyroid is suppressed by this hyperfunctioning nodule
· Adenomatous Hyperplasia
· Compensatory Hypertrophy - Such hypertrophy is seen when there is widespread damage to the gland (Hashimoto's).
· Physiologic Thyroid Hyperplasia - Patients who have congenital lobar agenesis (more commonly the left lobe [80%]), or are post surgical lobectomy, may appear to have a hot nodule which is suppressing the remainder of the gland.
·
Thyroid Carcinoma EXTREMELY
RARE . The probability of
cancer in a hot nodule scanned with radioiodine in less than 4%
q Indeterminate Nodule
o A thyroid suppression test may be performed to determine if the nodule is autonomous or cold. Cold nodules require further evaluation to exclude malignancy.
q Discordant Nodule
o Hot on Tc-99m images, but cold on the I-123 exam.
o Solitary discordant thyroid nodules are generally considered to be rare (2 to 8%) and cases of discrepancy between the Tc-99m and I-123 studies appear most often in multinodular goiters
o Discrepancies are also far more likely to be caused by benign thyroid disorders rather than malignancy [2,6].
o re-scan any patient with a hot nod
· Precautions While Using This MedicineReturn to top
q I-131 – precautions
o
Whether I-123 or I-131, should never be used
in a patient who is pregnant or nursing.
o No special precautions when this medicine is used in very small doses to help study the function of the thyroid.
o If for overactive thyroid or cancer of the thyroid
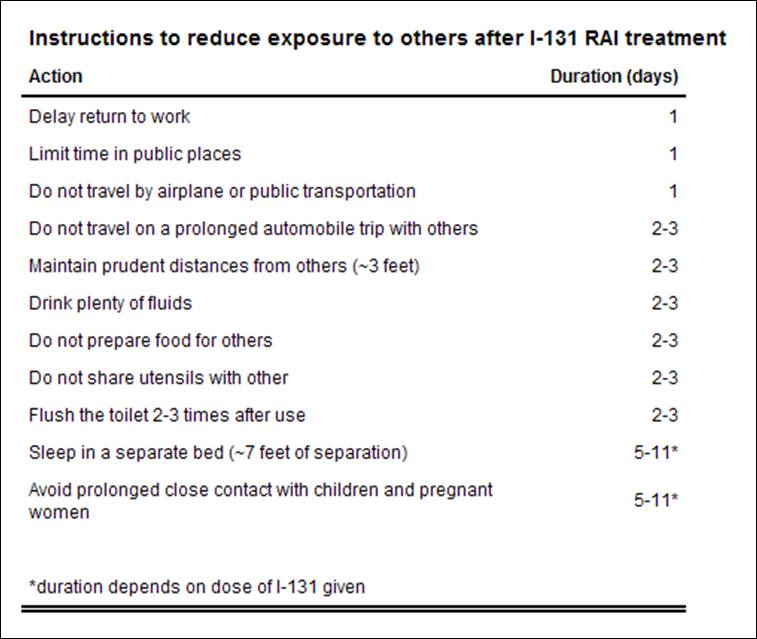
Figure 22 - I 131 - Precautions
q Radiotherapy In Non-Neoplastic Thyroid Disease
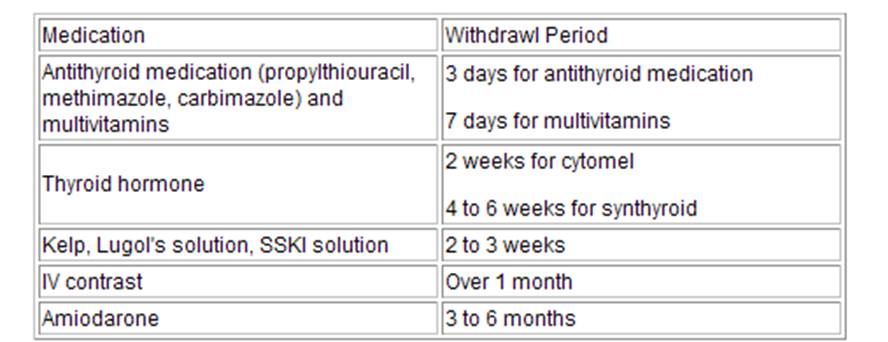
Figure 23 - Certain agents need to be discontinued prior to therapy
o
Contraindications to I-131 therapy
· Pregnancy: Radioiodine freely crosses the placenta.
· Breast feeding: Both iodine and pertechnetate are excreted in breast milk
· Severe thyrotoxicity: Patients should be pretreated (with beta-blockers) to avoid thyroid storm which can occur from sudden release of hormones following radiation destruction of the thyroid follicles
o
Standard dose of between 8 to 12 mCi, graves may need higher
dose, Nodules require higher dose upto 29.9mCi
o No significant change in thyroid function can be expected for 3 to 6 weeks.
o The maximum effects of the therapy should occur between 3 and 4 months.
o
Side Effects
· A transient sore throat or mild dysphagia.
· rare temporary thyrotoxicosis (or thyroid storm) thyroid storm is usually between 3 - 15 days after treatment, potentially fatal complication..
· Ophthalmopathy may develop after therapy [10].
· Risk of leukemia or other malignancy is no greater than in the general population. Additionally, there has been no demonstrable harmful effect upon the health of progeny, fertility, or reproductive history.
· No significant genetic effect has been demonstrated as well.
·
Nonetheless, women should be advised to
refrain from becoming pregnant for at least 6 to 12 months following therapy.
q I-131 imaging
o Whole-body imaging after a therapeutic dose of I-131 is the most sensitive means for localizing residual, recurrent or metastatic thyroid cancer, for those tumor types that are typically iodine avid (follicular and papillary carcinomas).
o Diagnostic I-131 imaging studies obtained after administration of 2-5 mCi are less sensitive because they are realtively counted limited
q Pet and thyroid cancer
o PET is being employed currently in the follow up of patients with thyroid cancer with rising thyroglobulin levels after thyroidectomy, following a negative I-131 whole body exam
o Thyroglobulin normally is made only in the thyroid
· serves an important function in the synthesis of thyroid hormone produced by the thyroid gland
q Pediatric Thyroid Cancer
o Less than 10% of papillary and follicular thyroid cancers occur in pediatric patients.
o f>m
o
The
therapeutic approach to thyroid cancer in children is identical to that in
adults- it includes surgery, radioactive iodine ablation, and TSH suppression with exogenous thyroxine.
q Papillary Thyroid Carcinoma (Roughly 66% of thyroid cancers)
o Both pure papillary tumors and those lesions that contain both papillary and follicular elements ("mixed" tumors)
o Papillary carcinoma is the most common thyroid cancer accounting for 50-89% of cases
o Females are affected more commonly than males. The mean age for patients to present is about 45.
o The majority of tumors are unilateral (70-80%), but can be multifocal in up to 25% of patients.
o In general, papillary cancers tend to be slow growing and there is about 93-97% long term survival (25 years) in patients who have complete surgical resection of the tumor and no evidence of metastatic disease.
o This is significantly better than survival in patients with follicular thyroid cancer.
o Lymphangitic spread to local neck nodes is most commonly seen and such regional nodal mets are found in 30 to 50% of patients at the time of diagnosis. The presence of initial local nodal mets does NOT influence survival, but does increase the risk for recurrenc.
o Distant mets is uncommon with the most common site for distant metastatic disease is the lung.
o The presence of mets in distant sites other than the lungs (bone, liver, brain) is an unfavorable prognostic variable in patients with documented lung mets.
q Follicular Thyroid Cancer (10-20% of thyroid cancers)
o carcinoma tends to occur in a slightly older age group (50 years) than papillary cancer and have an overall worse survival rate [10].
o Hematogenous distant metastases are seen
o The most common location for metastases is the lungs (70%), followed closely by the bones (65%), and also the brain (20%).
o Regional nodal metastases are found in only about 10% of patients.
o The overall mortality from follicular thyroid cancer is about 20%,
o Follicular neoplasms will usually concentrate technetium pertechnetate, but may not concentrate I-131- producing a "discordant nodule".
q Hurthle cell carcinoma
o is a follicular variant and it accounts for less than 10% of thyroid carcinomas.
o Most do NOT accumulate radioiodine (non-functional), but are capable of synthesizing thyroglobulin.
o Metastases can be either lymphatic or hematogenous.
o These patients have an overall worse prognosis
o On scintigraphy, both Thallium and Tc-Sestamibi have been shown to localize in recurrent tumor. FDG PET imaging is very good for imaging Hurthle cell neoplasms as intense tracer uptake is generally seen
q Anaplastic/Poorly Differentiated: (5%)
o Anaplastic carcinoma is usually seen in older patients (60-70y).
o The lesions typically do not concentrate iodine and the prognosis is poor.
q Medullary Thyroid Carcinoma
o Arises from the parafollicular C-cells and accounts for only 1 to 5% of all thyroid malignancies.
o The mean age at presentation is 60 y.
o These tumors may actively secrete calcitonin- a hormone involved in calcium homeostasis.
o Associated with MEN syndrome IIa and
o On scintigraphy medullary carcinoma appears as a cold nodule on routine thyroid scanning.
o I-131 MIBG has been used to image medullary carcinoma, but with only limited success.
o In-111 Octreotide (a somatostatin analog) has also been demonstrated to accumulate within the tumor, but the sensitivity is only about 50% (See also In-111 Octreotide Tumor Imaging).
q Primary Thyroid Lymphoma
o Rare
o It is seen more commonly in women than in men [8].
o It usually presents as a rapidly enlarging goiter.
o An increased risk for thyroid lymphoma is seen in patients with chronic lymphocytic thyroiditis [8].
o Thyroid lymphoma does not concentrate radioiodine.
q I-131 Ablation for Thyroid Neoplasms
o
Indications
· Thryoid remnant ablation: To destroy the small amount of thyroid tissue remaining in the neck after surgery
· For the treatment of functional metastases
· For the treatment of recurrent thyroid cancer
· For the treatment of patients with elevated thyroglobulin levels, but a negative I-131 scan
o
Treatment Protocols for Thyroid Carcinoma
· Residual thyroid bed activity only: 100 mCi
· Regional Metastases (Cervical Nodes): 150-175 mCi
· Lung Metastases: 175-200 mCi
· Skeletal Metastases: 200 mCi
o Acute Complications of I-131 Thyroid Ablation Therapy
· Sialoadenitis
· Loss of taste (Acute/Chronic)
· GI symptoms Nausea and vomiting (seen in <1%)
· Minimal bone marrow suppression
· Thyroid storm
o
Chronic Complications
· relative risk approximates 1.9 compared to the general population
q Tc99m Sestamibi
o Demonstrates slower washout from parathyroid adenomas and hyperplastic tissue compared to thyroid tissue.
o Adenoma detection (sensitivity of 90%) is more accurate than hyperpalstic.
o Some parathyroid adenomas demonstrate rapid release of Tc-sestamibi and may only be apparent on the early images.
o Dose 20 mCi
o
Image at 15 min and 2 hrs.
o uptake within a thyroid adenoma or thyroid carcinoma, or a cervical lymph node can produce a false-positive exam
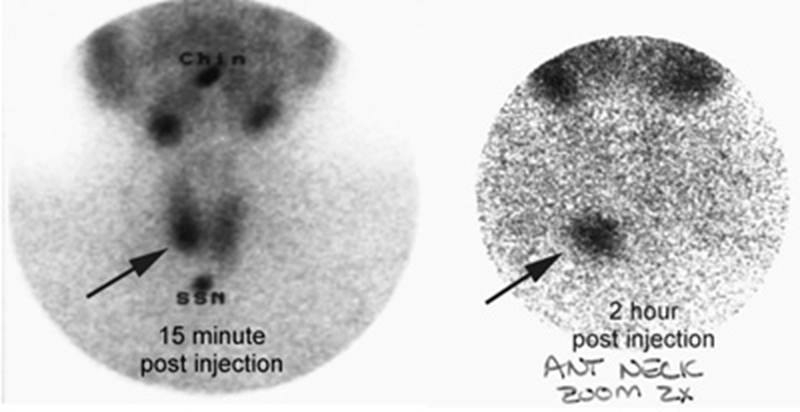
Figure 24 - Parathyroid adenoma
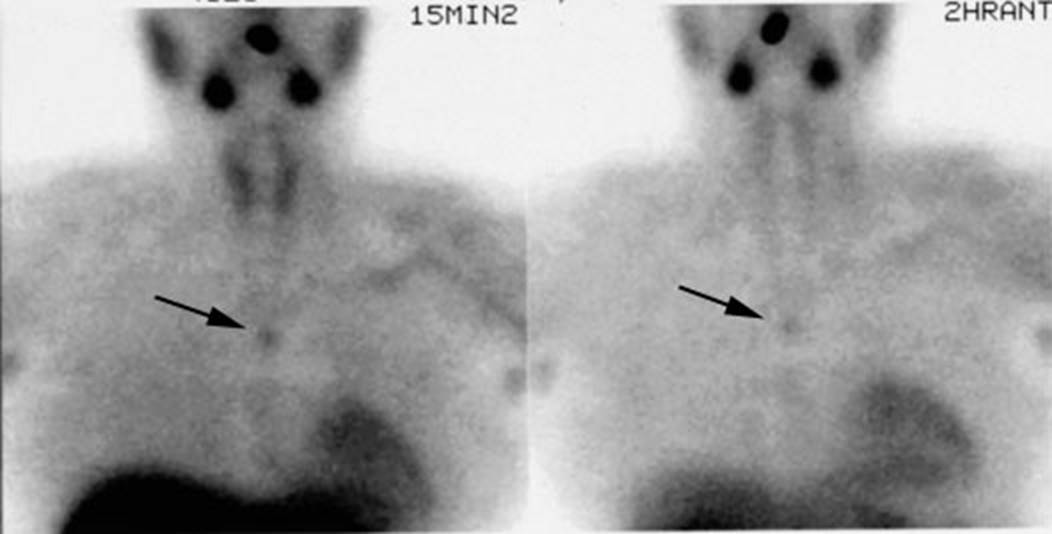
Figure 25 - Ectopic Parathyroid adenoma
q Other
o More traditional imaging uses Tc-99m pertechnetate and Tl -201 subtraction.
o Tl-201 accumaltes in both thyroid and parathyroid tissue and Tc 99m only accumaltes in thyroid.
o Typically Tl -201 is given 1st because lower energy, then patient given 1-2 mCi of pertechnetate and imaged at 10 minutes.
CNS Scintigraphic Imaging
q Blood brain Barrier
o Agents will cross when BBB is disrupted
o Best agents are Tc 99m DTPA and Tc-99m GH
o
Conventional brain scintigraphy is no longer
routinely performed
o
Methodolgy
·
Dynamic flow images are obtained, certain
disease stroke, AVM and Carotid
occlusion can be seen
· Usually performed in Anterior view
· Delayed planar images at 1 ½ to 2 hrs
o Normal cortex is devoid of activity, peripheral activity is scalp and meniges
o
Brain Tumors
· Less than 2 cm may be missed
· Menigioma and malignant gliomas are detected with high sensitivity, pituitary, parasellar and low grade gliomas are not.
· Donate shape, delayed uptake non specific, Stroke, abesss, mets can look similar.
o
Carotid Stenosis
· With high grade "Flip-Flop Phenomenon" is
seen in CVA's due to delayed arrival of radiotracer at the site of an infarct
via collateral vessels coupled with delayed washout from this area. This
finding may also be seen with high grade carotid artery stenosis without
infarction. The sign is characterized by:
· - Decreased arterial perfusion
- Equalization of activity during the capillary phase
- Increased activity in the dynamic
(venous) phase compared to the normal side.
o
Inflammation:
·
Blood flow is invariably increased to
inflammatory lesions.
·
Abscesses show increased activity on delayed images, and may have a "doughnut" appearance.
·
Again, these findings are not specific and may
be seen with neoplasms and rarely infarction.
·
Herpes encephalitis will demonstrate
increased flow and increased uptake on delayed images within the temporal lobe.
· Ventriculitis shows a pattern of bilateral increased lateral ventricle activity.
q PET
o F-18 FDG – gets phosphorylated and trapped intracellularly, good for cerebral metabolism
o Peak uptake at 35 minutes
o Uptake in gray matter is 3-4 times that of wm
o Increased uptake is seen with tumors and posticatal
o Decreaed uptake is seen in stroke and organic dementia
q SPECT Brain Perfusion Scintigraphy
o Tc99m-HMPAO (Hexamethylpropylenamine oxime): Ceretec
·
lipophilic compound
·
crosses the intact blood brain barrier by
passive diffusion. There is prompt CNS
uptake with peak activity occurring within 1 to 2 minutes after, then wash out
over 10-15 min
· activity which remains is then fixed in the brain via conversion to a hydrophilic compound by glutathione that cannot diffuse back out of the cell (intracellular oxidation of HMPAO by glutathione traps it inside the neurons and glial cells).
·
Activity
persists without washout for up to 24 hours
q Alzheimer's Dementia:
o Dementia affects 10% of people over the age of 60 years and Alzheimer's accounts for roughly 50% of these cases.
o Dementias produce deficits in perfusion, in part reflecting decreased metabolic needs.
o In Alzheimer's one classically sees bilateral decreased metabolism (PET imaging) and flow (SPECT imaging) in the temporal and parietal lobes with sparing of the primary motor, sensory, and visual cortices.
o Typically symmetrical (although symmetric, the defects are not necessarily of the same magnitude and severity.
o This pattern has a predictive value of over 80% for the diagnosis of Alzheimer's disease.
o
A correlation
has also been described between the severity of these defects, and the severity
of the patient's dementia.
o Unilateral temporoparietal or isolated frontal defects can be found seen early in the disease process.
o Overall, Tc99m-HMPAO imaging has a sensitivity between 80-90% and a specificity between 65-87% for the diagnosis of Alzheimer's dementia.
o The negative predictive value of a normal study is approximately 80% [1,2]. In one study which compared SPECT exam findings with autopsy results, SPECT imaging had a
o
Other disorders to be considered in the
differential of biparietal/temporal defects include:
Parkinson's disease with dementia, bilateral parietal infarcts, multi-infarct
dementia (typically asymmetric, and multiple small cortical defects),
hypoglycemia, and carbon monoxide poisoning.
q Parkinson's Disease:
o Parkinson's is a progressive neurodegenerative disorder resulting from the progressive death of dopaminergic neurons in the nigrostriatal pathway [5].
o Approximately 10% of patients affected with Parkinson's disease will develop dementia Generally, the perfusion pattern in these patients in non-specific and demonstrates either normal or mild global cortical deficits.
o
A pattern of bilateral posterior
parietal/temporal defects indistinguishable from Alzheimer's may be observed in
patients with Parkinson's disease with dementia
q Multi-infarct Dementia:
o Step-wise deterioration in intellectual function.
o MID is the second most common cause of dementia in the elderly [2].
o HMPAO findings that suggest the diagnosis include multiple, bilateral, and randomly distributed cortical perfusion defects that follow vascular territories.
o The basal ganglia, motor, and sensory cortices may also be involved (spared in Alzheimer's).
o Ischemic brain disease refers to dementia secondary to ischemia without evidence of frank infarction.
o The Diamox challenge test can be used to identify areas of perfusion abnormality in these patients as their baseline exam is often normal.
q HIV:
o
AIDS dementia complex (ADC ) can be seen in up to 11 to 65% of HIV
patients.
o Multiple areas (small and large) of decreased perfusion are identified in the cortical and subcortical regions, often producing a patchy distribution of the tracer.
o asal ganglia involvement is also common.
o
Scintigraphic findings similar
to ADC have also been
described in cocaine polysubstance drug abusers, Lyme disease, and chronic
fatigue syndrome.
q Pick's Disease (Frontal lobe dementia):
o Rare frontal dementia characterized by bilateral cerebral degeneration with atrophyaffecting the frontal or temporal lobes and involving both gray and white matter .
o SPECT images demonstrate bilateral, diffuse decreased frontal lobe perfusion extending to the cingulate gyrus
q Progressive supranuclear palsy:
o Will also produce decreased activity within the frontal lobes.
q Huntingtons
o
Huntingtons
o Brain SPECT imaging will demonstrate decreased or absent tracer uptake in the caudate or basal ganglia
o The defects are usually bilateral, but are not necessarily symmetric
q Korsakoff's Syndrome:
o Seen in alcohol abusers, it is due to thiamine deficiency. Perfusion defects tend to involve the posterior cortical regions predominantly.
Brain SPECT for the Detection of a Seizure focus:
q Partial Complex Seizures/Temporal Lobe Epilepsy:
o Epilepsy is one of the most prevalent neurological disorders- affecting about 1% of the general population .
o Seizures can be classified as either partial (focal) or generalized.
o Partial seizures originate in a given area of the brain and can be divided into simple (with no impairment of consciousness) and complex (with impairment of consciousness).
o Patients unresponsive to anti-convulsant therapy may be surgical candidates which can render the patient seizure free.
o Scalp EEG often fails to accurately localize the seizure focus and although depth EEG is much more accurate, it is also extremely invasive and suffers from regional under sampling.
o Most partial complex seizures originate in the temporal lobe.
o The most common pathologic finding in these patients is mesial temporal sclerosis which is thought to represent a gliotic scar.
o Excision of this focus can lead to elimination of the seizures or significantly improved pharmacologic control in 80% of patients.
q Ictal Imaging:
o The ictal exam requires that the patient be placed in a special room with continuous video and EEG monitoring.
o The patients medication is usually tapered off or discontinued to increase the likelihood of a seizure episode [2]. The tracer to be used is placed by the patients bedside and is already labeled.
o During the ictal phase of a complex partial seizure, there is typically hyperperfusion of the mesial or lateral aspects of the affected temporal lobe.
o Tc99m-HMPAO of Tc-99m ECD injected during the ictal state or in the immediate post-ictal period (within 30 to 60 seconds) will show a focal area increased activity (hypermetabolic region) at the seizure focus in 80 to 100% of patients.
o Crossed cerebellar hyperperfusion can also be identified in 75% of patients [10]. Ipsilateral or diffuse cerebellar hyperperfusion may also be seen [11].
o Ipsilateral basal ganglia hyperperfusion is also common [11].
o The injection should be performed before the seizure becomes generalized as identification of the seizure focus may not be possible should this occur .
o Early post-ictal scans (injection within minutes [1 to 10 minutes] following seizure termination) can demonstrate mesial hyperperfusion and/or lateral temporal hypoperfusion on the side of the seizure focus.
q Inter-ictal Imaging:
o Following the seizure, there is relatively rapid progression (generally within 20 minutes) to a hypoperfused state which persists throughout the inter-ictal phase.
o Inter-ictal (seizure free) SPECT studies will demonstrate an area of diminished tracer activity at the seizure focus in up to 50% of patients.
o
Inter-ictal PET FDG studies demonstrate a focal
area of hypometabolism in 60 to 70% of patients with normal MRI 's [1,2,3].
o The area of hypometabolism is often much larger than the actual area of structural abnormality.
o Both HMPAO and ECD are equivalent for localization of a seizure focus .
o A combination of hypoperfusion in the interictal study followed by hyperperfusion in the same region on the ictal exam has absolute specificity .
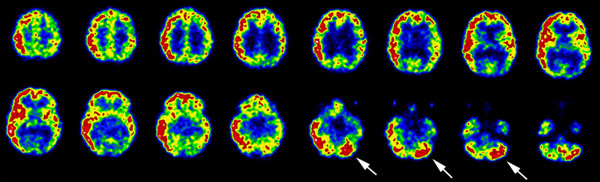
Figure 26 - Crossed cerebellar hyperperfusion (diaschisis): The ictal-SPECT exam below demonstrated extensive hyperperfusion (metabolism) involving a large portion of the right cerebral hemisphere. Crossed cerebellar hyperperfusion (white arrows) was also demonst
q Frontal Lobe Epilepsy:
o In the evaluation of frontal lobe epilepsy, SPECT images performed following the injection of Tc99m-HMPAO during the ictal period, demonstrated a hypermetabolic/hyperperfused seizure focus in 90% of cases.
o Inter-ictal SPECT imaging detected a hypoperfused seizure focus in only 11% of patients and therefore, interictal scanning is probably only useful in serving as a baseline exam. [3]
q Status Epilepticus:,
o ictal SPECT studies have demonstrated focal hyperperfusion in areas concordant with that suggested by EEG.
o Status epilepticus produces long term changes in regional cerebral blood flow that are not evident following a single seizure.
o As a result of this, persistent hyperperfusion may be observed for a prolonged period of time (possible out to 6 days following the event).
q Brain Tumors
o
Tc99m-HMPAO Imaging in Brain Tumors
·
Increased activity within certain lesions is
likely related to increased flow to the lesion given that Tc99m-HMPAO is a
perfusion agent.
· Increased uptake in meningiomas when compared to gliomas (except calcified meningiomas which have decreased uptake).
·
Within gliomas, regional tracer uptake increases
in relationship to the grade of malignancy [5], with low grade (I and II)
lesions demonstrating less uptake than grade III
tumors.
· Uptake within grade IV tumors tends to be mixed (high and low uptake zones) due to the presence of necrosis within the lesion.
·
Metastatic CNS
neoplasms generally demonstrate decreased tracer uptake, the exception to this
being renal cell carcinoma.
· Post-op gliosis can demonstrate increased Tc99m-HMPAO accumulation compared to the surrounding nonaffected brain tissue, although the uptake is generally not greater than that in the cerebellum
o
Thallium
· Uptkae in gliomas corresponds to higher grade
·
T1 201 and PET will avidly be taken up in lymphoma,
unlike infection
q CSF Flow Studies:
o CSF flow studies are performed using either In-111 (DTPA) or Tc99mDTPA.
o Indications for the exam include suspected normal pressure hydrocephalus, occult CSF rhinorrhea/otorrhea, and ventricular shunt evaluation.
q Radionuclide Shunt Scintigram:
o Radionuclide shuntograms have been used as an adjunct to aid in evaluation of shunt malfunction.
o Shunt complications include:
· Ventricular catheter blockage (most common)
· CSF loculation at the catheter tip:
· The lesion occurs secondary to adhesions and results in enlarging abdominal mass (CSFoma). Scintigraphic findings include focal pooling of tracer in the abdomen. To treat, the shunt is externalized, antibiotics instituted, and the collection should reabsorb on its own.
· Infection: Meningitis, ependymitis, abscess
· Subdural hematoma: Bridging veins in the subdural space may be torn with rapid decompression of hydrocephalus. This is generally a bilateral phenomenon.
· Craniosynostosis
· Aqueductal stenosis: Probably due to inflammation and results in non-communicating hydrocephalus.
· Thromboembolism: With cardiac atrial shunts
o Exam:
· Tc99m-DTPA or Tc99m-Human Serum Albumin (1 mCi) are the commonly used agents. In-111 DTPA (0.15-0.2 mCi) can be used when longer imaging times may be required. Agent is injected into the shunt reservoir and reflux of the agent into the ventricle is attempted..
· The patient is imaged for 30 minutes. Activity should rapidly clear from the ventricle (15-30 min.) and should pass through the shunt tubing into the abdomen.
· If no migration of activity is observed after 30 minutes, the patient should be placed in a sitting position and reimaged.
· Images over the abdomen should demonstrate free dispersion of the tracer throughout the peritoneal cavity.
· Renal and bladder activity will be seen as a result of peritoneal absorption of the tracer.
o Although the absence of ventricular reflux is a highly reliable indicator of proximal obstruction, a misdiagnosis rate of between 25-40% has been reported.
q Radionuclide Cisternography
o For the exam 250-500 uCi of In-111-DTPA is given intrathecally (Tc99m-DTPA may be adequate in children who have more rapid transit of the CSF if imaging will not be required beyond 24 hours).
o In adults activity is normally seen at the basal cisterns between 1 and 6 hours after injection.
o
Tracer activity should be at the frontal poles,
interhemispheric, and Sylvian fissures by 2 to 6 hours- producing a "Neptune 's trident" appearance.
o Activity should be at the cerebral convexities by 12 to 24 hours (no later than 48 hours) and the arachnoid villi in the sagittal sinus by 24 hours.
o There should be no or only minimal lateral ventricular activity seen since physiologic flow is in the opposite direction.
o Ventricular activity may be noted transiently in older patients between 12 and 24 hours.
o In young children tracer activity will reach the basilar cisterns in 30 minutes.
o Retrograde filling of the ventricular system is most likely to occur between 1 and 4 hours following injection.
q Normal Pressure Hydrocephalus (NPH):
o Image a 3 hrs – basal cisterns
o 24 and 48 – evaluation of ventricle reflux
o clinical triad of mental status changes, incontinence, and ataxia, with hydrocephalus and normal CSF pressures.
o The scintigraphic examination demonstrates a slow ascent over the convexities with little activity seen over the vertex.
o Ventricular reflux with delayed clearance of ventricular activity is also seen.
o Late intracerebral activity can be seen and is secondary to transependymal uptake of the tracer.
o Surgical shunting of CSF can potentially reverse this progressive disorder.
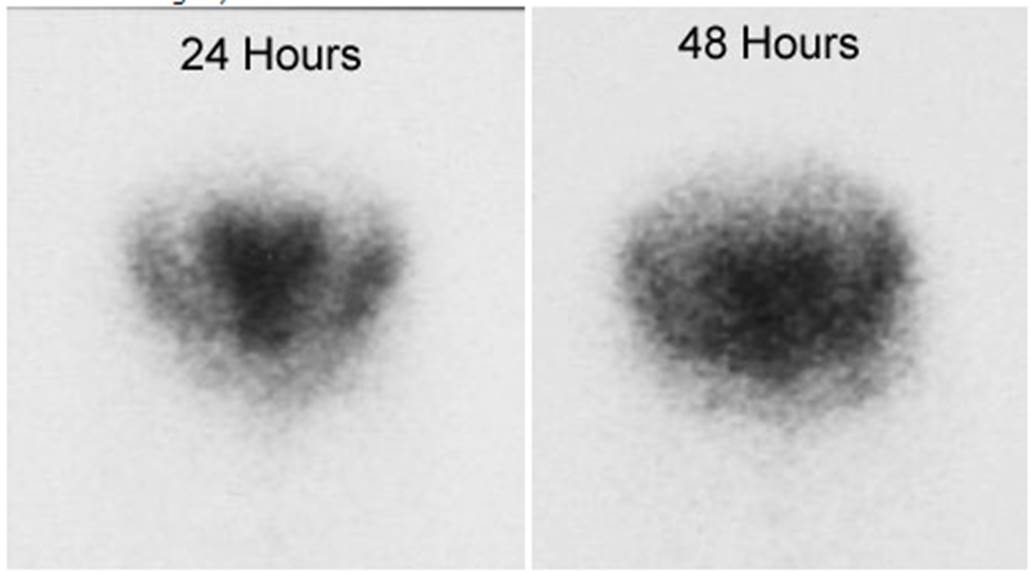
Figure 27 -
q Communicating Hydrocephalus:
o Refers to an extraventricular obstruction in the basal cisterns, cerebral convexities, or arachnoid villi.
o Etiologies include a previous subarachnoid hemorrhage, meningitis, or leptomeningeal carcinomatosis.
o On scintigraphy, there is delayed flow over the convexities and reflux of activity into the ventricles with marked, persistent ventricular activity out to 72 hours.
o Differentiation from NPH is based upon clinical findings.
q CSF Leak Study:
o
Pledgets placed by ENT
or Neurosurgery in the anterior and posterior portion of each nasal region.
o The pledgets are left in for 24 hours.
o It is often useful to have the patient in the position which is associated with the greatest leakage during this time (images should also be acquired in this position).
o Children may not tolerate the packs for more than a few hours. They can be placed 30 minutes after injection and removed after 4 to 6 hours if necessary.
o Counts are collected in a well counter.
o A ratio of nasal to plasma radioactivity greater than 1.3:1 is considered positive for a leak.
q Flow
q Acetazolamide (Diamox) challenge test
o Used to assess cerebral perfusion reserve.
o
The exam may be useful in identifying CNS territory at risk in patients experiencing
TIA's and for patients being considered for carotid ligation surgery.
o Acetazolamide is a carbonic anhydrase inhibitor that causes an increase in cerebral CO2. This results in vasodilatation and increased flow in normal cerebral vessels.
o In an area of reduced blood flow, where there has already been maximal vasodilatation (and thus loss of cerebrovascular reserve) there can be no augmentation of flow.
o To perform the study, a baseline exam is compared to a SPECT exam performed 25 minutes after the I.V. administration of 1 gm of acetazolamide given over 2 minutes (peak pharmacologic action is seen about 20-25 minutes after IV administration and the agent has a half-life of about 90 minutes- blood flow returns to normal between 2-3 hours after injection) [12,16].
o Areas of limited flow reserve will have decreased tracer activity on the challenge exam compared to the baseline study .
o A decrease of 10 to 20% in activity on the Diamox exam compared to baseline is considered abnormal.
o
The exam has also been performed using both
Tc99m-HMPAO and I-123 IMP
o The challenge test is not without limitations.
q Brain Death:
HMPAO is taken up by normal, viable brain tissue with no significant redistribution- this makes the agent particularly helpful in cases of suspected brain death.
SPECT imaging in patients with brain death demonstrates no cerebral or cerebellar accumulation of the radiotracer.
Figure 28 - Brain death: Coronal images from a Tc-HMPAO examination demonstrate no uptake of tracer by the brain parenchyma consistent with brain death.